If you’re reading this guide, you’re likely facing one of life’s most challenging moments – receiving news that you need medical intervention for a lung-related condition. The words “pleural biopsy” or “pleurodesis” may have left you feeling overwhelmed, scared, or uncertain about what lies ahead. Please know that what you’re feeling is completely natural, and you are absolutely not alone in this journey.
This comprehensive guide has been written with a deep understanding of the emotions, questions, and concerns you’re experiencing right now. We’re here to walk alongside you, providing not just medical information but genuine support, hope, and practical guidance that will empower you to make the best decisions for your health and well-being.
Take a moment to breathe deeply. You’ve already taken the most important step by seeking information and advocating for your health. That courage and determination will serve you well throughout this process.
Understanding Your Situation: You’re Stronger Than You Know
Receiving a recommendation for pleural procedures can feel like your world has been turned upside down. One day, you might have been going about your normal routine, and the next, you’re faced with medical terminology that sounds foreign and frightening. This emotional whirlwind is completely understandable – you’re processing not just medical information, but also fears about your future, concerns about your loved ones, and questions about what this means for your life.
In patients with malignant pleural effusion, these procedures have helped countless individuals reclaim their health and quality of life. Every day, people just like you undergo these treatments and return to the activities, relationships, and dreams that matter most to them.
What Are Pleural Procedures Really About?
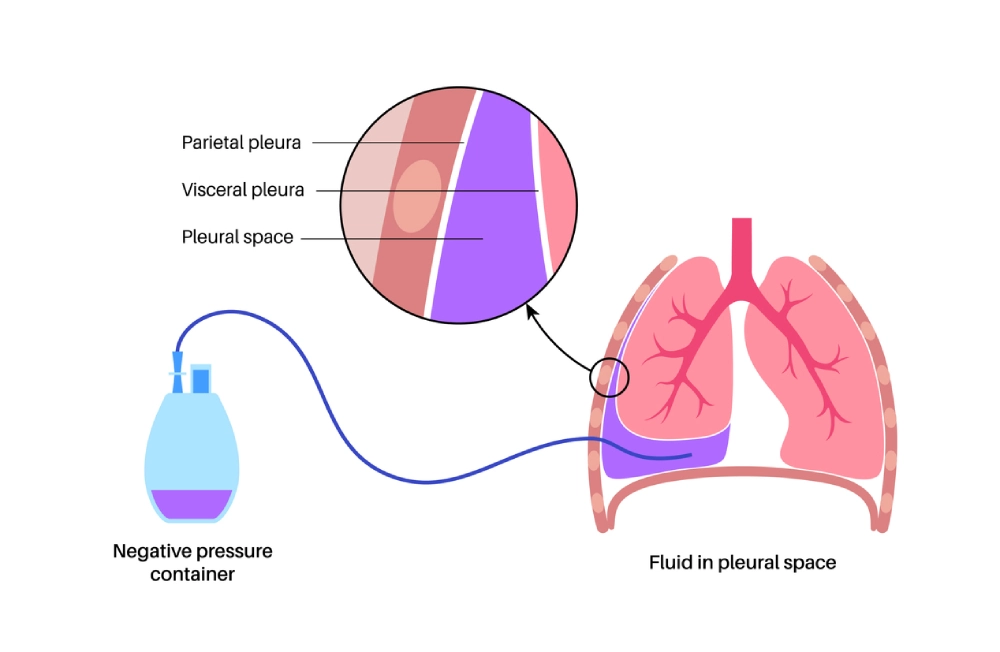
Your lungs are remarkable organs, protected by a delicate, thin membrane called the pleura. Think of the pleura as a gentle, protective embrace around your lungs – two smooth layers that allow your lungs to expand and contract effortlessly with each breath. When something affects this area, it can impact your breathing, comfort, and overall well-being.
Sometimes, pleural fluid accumulates in the space between the lung and the chest wall, known as the pleural cavity or chest cavity. You can think of it as a box where normally a balloon full of air (the lung) touches the inside of the box. If you pour water in the box, the balloon becomes smaller and won’t inflate as well.
Pleural Biopsy: Your Path to Answers and Peace of Mind
Understanding What a Pleural Biopsy Really Means
When your doctor recommends a pleural biopsy, they’re essentially saying, “We want to gather the most accurate information possible so we can provide you with the best care.” This isn’t a sign that something terrible is happening – it’s a sign that your medical team is being thorough, careful, and committed to getting you the right treatment.
Pleural biopsy services are available in most major medical centers, and the procedure itself is far less intimidating than you might imagine. A pleural biopsy involves taking a tiny tissue sample from the pleura – think of it as gathering a small piece of the puzzle that will help your medical team see the complete picture of your health.
Why Your Doctor Recommends This Procedure
Your healthcare team doesn’t make recommendations lightly. When they suggest a pleural biopsy, it’s because they care deeply about providing you with accurate answers. Here are the most common reasons why this procedure might be recommended:
- Investigating Unexplained Fluid Buildup (undiagnosed Pleural Effusion): Sometimes fluid accumulates around the lungs, causing discomfort, breathlessness, or chest pain. A biopsy helps identify exactly what’s causing this fluid buildup, whether it’s an infection that can be treated with antibiotics (parapneumonic effusion), inflammation that responds to specific medications (recurrent pleural effusion), or another condition that requires targeted therapy. Sometimes fluid accumulation is caused by cancer, which we call malignant effusion.
- Lung Cancer Diagnosis and Staging: If there’s any concern about cancer, a biopsy provides definitive answers. While the word “cancer” naturally causes fear, remember that early detection and accurate staging are your greatest allies. Many lung cancers, when caught early, respond excellently to treatment. Fluid buildup can also be caused by malignant pleural mesothelioma, an incurable cancer of the lining of the chest wall.
- Ruling Out Serious Infections: Sometimes, what appears concerning on imaging studies turns out to be a treatable infection, such as tuberculosis. A biopsy can quickly identify these conditions, leading to targeted antibiotic treatment and complete recovery.
- Investigating Occupational Lung Diseases: For individuals with potential asbestos exposure, a biopsy can provide crucial diagnostic information about conditions like mesothelioma. Specialist teams who diagnose mesothelioma understand the unique concerns of patients with occupational exposures and provide both medical care and emotional support throughout the diagnostic process.
The Different Types of Pleural Biopsy: Finding the Right Approach for You
Advanced pleural biopsy techniques have evolved significantly, offering multiple approaches that prioritise your comfort and safety:
- Needle Biopsy (Percutaneous): This is often the first approach considered. Using advanced imaging guidance like ultrasound or CT scans, your doctor guides a thin needle to the precise location needed. Most patients are surprised by how manageable this procedure is – the needle is much smaller than they imagined, and local anaesthesia ensures comfort throughout.
- Thoracoscopic Biopsy: Sometimes called “keyhole surgery,” this minimally invasive approach uses a small, flexible tube with a camera. Minimally invasive thoracic surgery allows your surgeon to see exactly what they’re doing while making only tiny incisions. Recovery is typically faster and more comfortable than traditional open surgery.
- Video-Assisted Thoracoscopic Surgery (VATS): This represents the gold standard in minimally invasive chest surgery. This technique is often considered the standard approach when larger tissue samples are needed, while still maintaining the benefits of minimal invasiveness – smaller incisions, less pain, and faster recovery. The diagnostic yield of this procedure is much higher than that of any other technique in diagnosing any pleural abnormality.
What to Expect: Your Biopsy Experience Step by Step
Your care team will guide you through preparation well before the procedure day. Here’s what you can expect:
Your Initial Consultation: Your first meeting with your thoracic specialist is about more than just medical evaluation – it’s about building a relationship of trust and understanding. Compassionate thoracic surgeons take time to listen to your concerns, answer your questions, and explain everything in terms that make sense to you. Don’t hesitate to ask about your surgeon’s experience, success rates, and approach to patient care.
Pre-Procedure Preparation: You’ll receive detailed instructions about preparing for your biopsy. This typically includes:
- Medication review to ensure safety during the procedure
- Any necessary lab work or additional imaging studies should always include at least an up-to-date CT scan.
- Clear guidelines about eating and drinking before the procedure
- Arrangements for transportation home
- Information about what to wear and bring on procedure day
The Day of Your Procedure: Patient-centered biopsy services ensure your comfort from the moment you arrive. You’ll meet with your entire care team, have opportunities to ask final questions, and receive clear explanations about each step of the process. Most patients find that the anticipation is much worse than the experience.
During the Biopsy: The procedure typically takes 30-90 minutes, depending on the approach used. You’ll receive appropriate anaesthesia – either local anaesthesia for needle biopsies or sedation for thoracoscopic procedures. Expert anaesthesia services ensure you’re comfortable throughout the entire process.

Many patients report being surprised by how manageable the experience is. One patient shared, “I spent weeks worrying about the biopsy, but when it was over, I realised I had worked myself up over something that was actually quite tolerable. The team was so caring and professional – I felt safe throughout the entire process.”
Immediately After Your Procedure: You’ll be carefully monitored in a recovery area where nursing staff will check your vital signs and ensure you’re feeling well.
Comprehensive post-procedure care: Includes pain management, instructions for home care, and scheduling of follow-up appointments.
Pleurodesis: Your Solution for Recurring Lung Problems
Understanding Pleurodesis: A Life-Changing Treatment Option
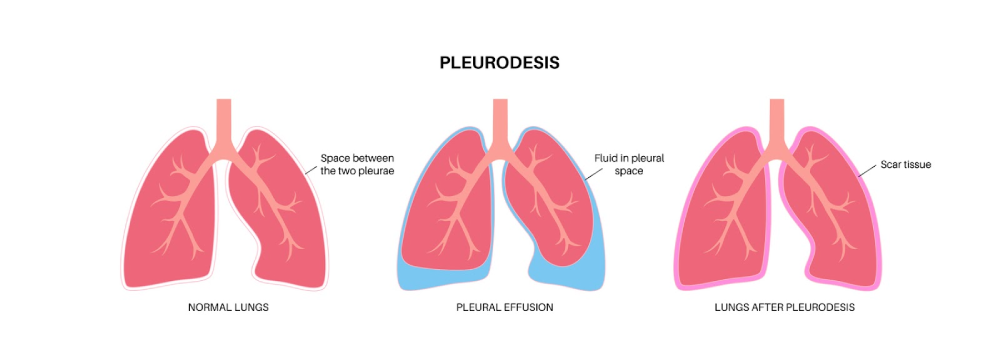
If you’re dealing with recurring pleural effusions (fluid buildup around the lungs) or repeated episodes of pneumothorax (collapsed lung), pleurodesis might be the definitive solution you’ve been hoping for. This procedure is designed to prevent future episodes by essentially “sealing” the pleural space.
Pleurodesis has helped many patients who previously struggled with recurring fluid or lung collapse. Pleurodesis offers the possibility of genuine freedom from these recurring problems.
How Pleurodesis Works
Pleurodesis works by creating a controlled, therapeutic inflammatory response that causes the two layers of the pleural tissue to adhere together. While the word “inflammatory” might sound concerning, this is actually a carefully orchestrated healing process that eliminates the space where fluid or air can accumulate.
Think of it like this: imagine having a space between two surfaces where water keeps collecting. Pleurodesis essentially eliminates that space by bringing the surfaces together, preventing future water accumulation. Pleurodesis is performed using well-established techniques that have been refined over decades.
Types of Pleurodesis: Choosing the Best Approach for Your Situation
Personalised pleurodesis treatment plans take into account your specific condition, overall health, previous treatments, and personal preferences. Your thoracic specialist will work with you to determine the best approach:
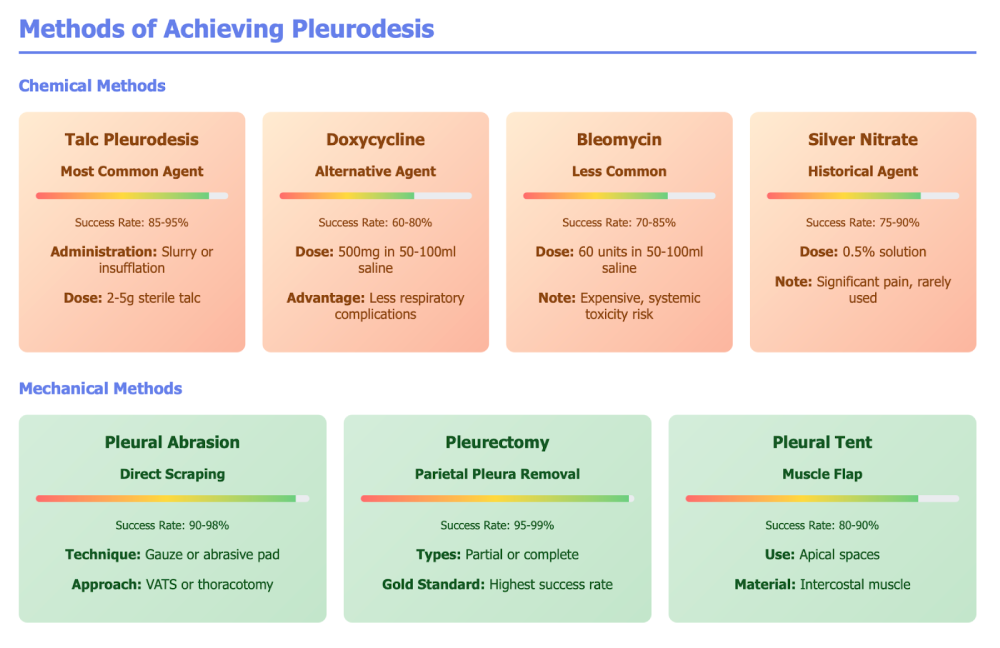
- Chemical Pleurodesis: This approach uses safe, effective medications to create the desired pleural adhesion. Professional chemical pleurodesis services typically use one of several proven agents:
- Talc Pleurodesis: The most commonly used and effective option, with success rates often exceeding 90%. Medical-grade talc is completely different from cosmetic talc and has been safely used for pleurodesis for decades.
- Doxycycline Pleurodesis: An antibiotic that also has sclerosing properties, sometimes chosen for patients with specific medical considerations.
- Bleomycin Pleurodesis: A medication that can be effective in certain situations, though less commonly used due to cost considerations.
Chemical pleurodesis can often be performed through a chest tube, making it a less invasive option for many patients.
Outpatient pleurodesis procedures are sometimes possible, depending on your specific situation.
Mechanical Pleurodesis: This surgical approach involves physically treating the pleural surfaces to promote adhesion. This procedure is performed by thoracic surgeons during thoracoscopy or thoracotomy, literally abrading or treating the pleural surfaces to encourage them to grow together.
Mechanical pleurodesis might be recommended when:
- Chemical methods haven’t been successful
- Your surgeon can address other issues simultaneously
- Your specific anatomy or condition makes a mechanical approach preferable
There are different ways to perform a pleurodesis:
- By the bedside, using a small amount of talc (otherwise very painful). The advantage is that it is quick and doesn’t involve any general anaesthetic or surgery, only a local anaesthetic. The disadvantage is that it is not that effective, and it is not possible to perform any sampling (either lung biopsy or biopsy of any pleural thickening).
- By medical thoracoscopy: it is done under deep sedation, almost like a general anaesthetic, but the patient breathes on his own. Better success rate, but still quite a high chance of recurrent malignant pleural effusion.
- VATs pleurodesis: this is the best way to achieve pleurodesis, the most successful, but it requires a general anaesthetic.
Please be mindful that pleurodesis is only possible if the lung expands fully. Imagine pleurodesis like gluing two things together; it is only possible if they touch each other. If the lung does not expand after pleural fluid drainage (we call it trapped), then we use a semipermanent indwelling pleural catheter. This is a very soft and small tube that doesn’t show underneath your clothes and connects to a special bottle to drain the fluid regularly at home. With ongoing pleural drainage, eventually over time, the space shrinks, and the catheter can be removed.


The Incredible Benefits: How Pleurodesis Can Transform Your Life
Successful pleurodesi recovery stories from patients describe improvements that extend far beyond just preventing fluid accumulation:
Restored Breathing Freedom: “I didn’t realise how much my breathing had been affected until after the pleurodesis,” shares one patient. “Suddenly, I could take deep breaths again without that constant feeling of pressure in my chest. It was like someone had lifted a weight off my lungs.”
Improved Sleep Quality: Many patients report dramatically better sleep after pleurodesis. Without the discomfort and breathing difficulties caused by pleural effusions, patients can finally rest peacefully through the night.
Reduced Anxiety and Worry: Perhaps one of the most significant benefits is psychological. Long-term pleural health management through pleurodesis eliminates the constant worry about when the next episode might occur. Patients describe feeling “free” from the fear that had been controlling their lives.
Increased Activity Tolerance: Simple activities like climbing stairs, carrying groceries, or playing with grandchildren become possible again. Enhanced quality of life after pleurodesis often exceeds patients’ expectations.
Fewer Medical Interventions: Instead of repeated procedures to drain fluid, pleurodesis offers a one-time solution that can prevent future episodes entirely. This means fewer hospital visits, fewer procedures, and more time living your life.
Choosing Your Medical Team: Partners in Your Healing Journey
Finding the Right Thoracic Specialist
Experienced thoracic surgeons combine technical skill with compassionate care. When selecting your medical team, consider these important factors:
Experience and Expertise: Look for surgeons who perform pleural procedures regularly. Board-certified thoracic surgeons have completed extensive training specifically in chest surgery and maintain ongoing education in the latest techniques and technologies.
Don’t hesitate to ask about your surgeon’s experience:
- How many pleural biopsies and pleurodesis procedures do they perform annually?
- What are their success rates?
- How do they handle complications if they arise?
- Can they provide references from other patients?
Communication Style and Bedside Manner: Patient-centered thoracic care means your surgeon takes time to listen to your concerns, explains procedures in understandable terms, and respects your questions and fears. You should feel comfortable asking anything, no matter how small it might seem.
Hospital Quality and Accreditation: Accredited hospitals follow strict quality standards for equipment, staffing, and safety. Look for hospitals with:
- Joint Commission accreditation
- Magnet status for nursing excellence
- High patient satisfaction scores
- Low infection and complication rates
- Advanced emergency response capabilities
Multidisciplinary Team Approach: Comprehensive lung care teams include not just surgeons, but also pulmonologists, oncologists (if cancer is a concern), specialised nurses, respiratory therapists, and social workers. This team approach ensures all aspects of your care are coordinated and optimised.
Understanding the Cost and Insurance Aspects
These procedures are generally recognised as medically necessary and often covered by insurance. However, navigating insurance can be complex during an already stressful time.
Insurance coverage for pleural surgery typically includes:
- Diagnostic procedures like biopsies
- Therapeutic procedures like pleurodesis
- Hospital stays and recovery care
- Follow-up appointments and monitoring
Financial assistance for lung procedures is often available through:
- Hospital charity care programs
- Payment plan options
- Patient assistance programs from pharmaceutical companies
- Non-profit organisations that support lung disease patients
Work with your healthcare team’s financial counselors to understand your specific coverage and explore all available options for making your care affordable.
Preparing for Your Procedure: Setting Yourself Up for Success
Physical Preparation
Pre-procedure optimisation can significantly improve your outcomes and recovery experience:
- Smoking Cessation: If you smoke, quitting before your procedure is one of the most important things you can do for your health. Smoking cessation support programs can provide medications, counseling, and resources to help you quit successfully. Even stopping a few days before your procedure can improve healing and reduce complications.
- Nutritional Optimisation: Good nutrition supports healing and recovery. Pre-surgical nutrition counseling might include recommendations for protein intake, vitamins, and minerals that support tissue repair and immune function.
- Exercise and Conditioning: If you’re physically able, gentle exercise before your procedure can improve your overall conditioning and make recovery easier. Even simple walking or breathing exercises can be beneficial.
- Managing Other Health Conditions: Work with your healthcare team to optimise management of other conditions like diabetes, heart disease, or high blood pressure. Comprehensive pre-operative care ensures all aspects of your health are considered.
Emotional and Psychological Preparation
Emotional support during lung procedures is just as important as physical preparation:
- Understanding Your Feelings: It’s completely normal to experience a wide range of emotions – fear, anxiety, sadness, anger, or even relief that you’re finally getting answers and treatment. There’s no “right” way to feel, and all of your emotions are valid.
- Building Your Support Network: Identify family members, friends, or support groups who can provide emotional support throughout your journey. Lung disease support groups connect you with others who truly understand what you’re experiencing.
- Stress Management Techniques: Learning relaxation techniques, deep breathing exercises, or meditation can help manage anxiety before and after your procedure. Integrative medicine for lung patients often includes these complementary approaches to healing.
- Spiritual Care: Many patients find comfort in spiritual support, whether through their own faith tradition or hospital chaplaincy services. Holistic lung care addresses not just your physical needs but your emotional and spiritual well-being as well.
Practical Preparations
Procedure day logistics require some planning:
Transportation Arrangements: You’ll need someone to drive you home after your procedure. Even if you feel fine, anaesthesia and medications can affect your reaction time and judgment for several hours.
Home Recovery Setup: Prepare your home for comfortable recovery:
- Set up a comfortable resting area on the main floor, if possible
- Stock up on easy-to-prepare meals
- Arrange for help with household tasks for a few days
- Ensure you have all prescribed medications
Work and Activity Planning: Most patients need several days to a week off work, depending on their job requirements and the specific procedure performed. Return to work after pleural surgery varies by individual, but your healthcare team will provide specific guidance.
The Recovery Journey: What to Expect and How to Thrive

Immediate Post-Procedure Recovery
Optimal pleural surgery recovery begins immediately after your procedure:
In the Hospital: You’ll be closely monitored by experienced nursing staff who specialise in caring for thoracic surgery patients. Post-operative care includes:
- Regular assessment of your breathing and comfort level
- Pain management tailored to your specific needs
- Monitoring for any signs of complications
- Gradual mobilisation to prevent complications and promote healing
Going Home: Most pleural procedures allow you to go home the same day or after an overnight stay. Safe discharge planning ensures you have everything you need for successful recovery at home.
The First Few Days: It’s normal to experience some discomfort, fatigue, and mild shortness of breath initially. Comprehensive discharge instructions will guide you through:
- Activity restrictions and gradual return to normal activities
- Wound care and monitoring for signs of infection
- Pain management strategies
- When to call your healthcare team with concerns
Managing Recovery Challenges
Successful recovery from pleural procedures involves understanding what’s normal and what requires medical attention:
Normal Recovery Experiences:
- Mild to moderate discomfort at incision sites
- Some fatigue for the first week or two
- Gradual improvement in breathing (this may take several weeks)
- Emotional ups and downs as you process your experience
When to Seek Medical Attention: Contact your healthcare team immediately if you experience:
- Severe or worsening chest pain
- Significant shortness of breath
- Signs of infection (fever, chills, unusual drainage)
- Severe nausea or vomiting
- Any symptoms that worry you
Long-Term Recovery and Monitoring: Follow-up care after pleural surgery is crucial for ensuring optimal outcomes.
Scheduled Appointments: Your surgeon will want to see you at regular intervals to monitor your healing and ensure the procedure was successful. Comprehensive follow-up care typically includes:
- Wound check within the first week
- Imaging studies to confirm successful healing
- Assessment of breathing improvement
- Discussion of any ongoing concerns
Lifestyle Modifications for Optimal Health: Healthy living after lung procedures can enhance your recovery and long-term well-being.
Pulmonary Rehabilitation: Professional pulmonary rehabilitation programs can significantly improve your breathing capacity, exercise tolerance, and overall quality of life. These programs typically include:
- Breathing exercises and techniques
- Gradual exercise conditioning
- Education about lung health
- Nutritional counseling
- Emotional support and coping strategies
Environmental Modifications: Simple changes to your environment can support your lung health:
- Avoiding exposure to irritants like smoke, strong chemicals, or pollution
- Using air purifiers if needed
- Maintaining good humidity levels in your home
- Regular cleaning to reduce dust and allergens
Ongoing Health Maintenance: Long-term lung health management includes:
- Regular follow-up with your pulmonologist or thoracic surgeon
- Staying current with vaccinations, especially flu and pneumonia vaccines
- Prompt treatment of respiratory infections
- Continued smoking cessation if applicable
- Regular exercise as approved by your healthcare team
Advanced Treatment Options and Emerging Technologies
Cutting-Edge Pleural Treatments
Innovative pleural procedure techniques continue to evolve, offering patients even better outcomes with less invasiveness:
- Robotic-Assisted Surgery: In some cases, robotic systems may be used, allowing surgeons to perform procedures with greater precision.
- Enhanced Imaging Guidance: Advanced imaging for pleural procedures includes real-time ultrasound guidance, CT-guided procedures, and even electromagnetic navigation systems that help surgeons locate target areas with millimeter precision.
- Improved Pain Management: Multimodal pain management for thoracic surgery uses combinations of medications and techniques to minimise discomfort while reducing dependence on opioid medications.
Personalised Medicine Approaches
Individualised pleural treatment plans take into account your specific genetic makeup, medical history, and personal circumstances:
- Biomarker Testing: For patients with pleural effusions, advanced diagnostic testing can identify specific biomarkers that help predict which treatments will be most effective.
- Precision Medicine: Personalised lung cancer treatment uses genetic testing of tumors to identify the most effective targeted therapies.
Research and Clinical Trials: Hope for the Future
Participating in Clinical Research
Clinical trials for pleural diseases offer access to cutting-edge treatments that aren’t yet widely available. Participating in research can provide:
- Access to innovative treatments
- Close monitoring by research teams
- Contribution to advancing medical knowledge
- Potential for better outcomes
Finding appropriate clinical trials involves working with your healthcare team to identify studies that match your specific condition and circumstances.
Future Directions in Pleural Care
Emerging pleural treatments on the horizon include:
- New sclerosing agents for pleurodesis with potentially better efficacy
- Improved surgical techniques that further reduce invasiveness
- Better understanding of genetic factors in pleural diseases
- Advanced imaging technologies for earlier detection and monitoring
Living Well After Pleural Procedures: Your New Chapter
Returning to Activities You Love
An active lifestyle after pleural surgery is not only possible but encouraged. Many patients find they can return to activities they thought they might never enjoy again:
- Exercise and Physical Activity: With proper healing and medical clearance, most patients can return to their preferred forms of exercise. Safe exercise after lung surgery guidelines help you gradually rebuild your strength and endurance.
- Travel and Adventure: Many patients wonder if they’ll be able to travel after pleural procedures. With proper planning and medical clearance, travel is usually possible. Travel considerations after lung surgery include timing, altitude considerations, and carrying medical documentation.
- Work and Career: Most patients can return to their careers, though some modifications might be needed initially. Workplace accommodations for lung patients can help ensure a smooth transition back to professional responsibilities.
Building Resilience and Finding Meaning
Emotional wellness after lung procedures often involves a process of finding new meaning and perspective:
- Post-Traumatic Growth: Many patients describe experiencing positive changes after going through medical challenges – increased appreciation for life, stronger relationships, clearer priorities, and greater resilience.
- Giving Back: Some patients find meaning in helping others going through similar experiences, whether through formal support groups, mentoring programs, or advocacy work.
- Mindfulness and Gratitude: Mindfulness practices for lung patients can help develop a greater appreciation for each breath and each day of improved health.
Your Support Network: You’re Never Alone
Professional Support Resources
Comprehensive lung disease support services include:
- Medical Social Workers: These professionals can help navigate insurance issues, connect you with community resources, and provide emotional support throughout your journey.
- Patient Navigators: Dedicated patient navigation services help coordinate your care, schedule appointments, and ensure smooth communication between different members of your healthcare team.
- Spiritual Care: Hospital chaplains and spiritual care providers offer support regardless of your religious background or beliefs.
Peer Support and Community
Lung disease community support provides a connection with others who truly understand your experience:
- Support Groups: Both in-person and online support groups connect you with others who have undergone similar procedures. Local lung disease support groups provide opportunities for face-to-face connection and shared experiences.
- Online Communities: Virtual support for lung patients includes forums, social media groups, and video support meetings that can be accessed from anywhere.
- Family and Caregiver Support: Resources for lung disease caregivers help your loved ones understand how to best support you while taking care of their own emotional needs.
Your Questions Answered: Comprehensive FAQ
Common Concerns About Pleural Procedures
Will I be able to breathe normally after the procedure?
Most patients experience significant improvement in their breathing after successful pleural procedures. While it may take several weeks to feel the full benefits, many patients report breathing better than they have in months or years.
How long will I need to stay in the hospital?
Many pleural biopsies are outpatient procedures, meaning you go home the same day. Pleurodesis may require an overnight stay or a few days in the hospital, depending on the specific technique used and your individual recovery.
What if the procedure doesn’t work?
While pleural procedures have high success rates, your healthcare team will discuss backup plans and alternative treatments. Secondary treatment options for pleural diseases ensure that you have multiple pathways to achieving relief.
Will I need ongoing medical care?
You’ll need regular follow-up appointments to monitor your recovery and ensure continued success. The frequency of these visits typically decreases over time as your condition stabilises.
Specific Procedure Questions
Is a pleural biopsy painful?
Most patients report that the pleural biopsy is much more tolerable than they expected. Local anaesthesia or sedation ensures comfort during the procedure, and any post-procedure discomfort is typically mild and easily managed.
How successful is pleurodesis?
Success rates for pleurodesis are generally very high, often exceeding 90% for preventing recurrent pleural effusions. Pleurodesis success rates vary slightly depending on the underlying condition and technique used.
What are the alternatives to these procedures?
Your healthcare team will discuss all available options, which might include medications, less invasive procedures, or watchful waiting, depending on your specific situation.
Taking Action: Your Next Steps Towards Healing

Scheduling Your Consultation
Expert pleural consultation scheduling is the first step towards getting the answers and treatment you need:
Preparing for Your First Appointment:
- Gather all relevant medical records and test results
- List all current medications and supplements
- Prepare a list of questions and concerns
- Bring a trusted friend or family member for support
- Write down your symptoms and when they started
Questions to Ask During Your Consultation:
- What is your experience with my specific condition?
- What are all my treatment options?
- What are the risks and benefits of each option?
- What can I expect during recovery?
- How will you monitor my progress?
- What support services are available?
Making the Decision
Informed decision-making for pleural procedures involves weighing multiple factors:
Medical Factors:
- Severity of your current symptoms
- Likelihood of symptom progression without treatment
- Your overall health status
- Previous treatment responses
Personal Factors:
- Impact on your quality of life
- Family and work responsibilities
- Personal preferences and values
- Support system availability
Practical Factors:
- Insurance coverage and financial considerations
- Geographic access to specialised care
- Timing considerations
Moving Forward with Confidence
Remember that choosing to proceed with pleural procedures isn’t just about addressing a medical condition – it’s about investing in your future, your relationships, and all the moments that make life meaningful. Confident healthcare decision-making comes from feeling informed, supported, and assured that you’re taking the right steps for your unique situation.
Conclusion: Your Journey to Better Health Starts Here
As we conclude this comprehensive guide, we want you to know that every word has been written with a deep understanding of what you’re going through and a genuine hope for your healing journey ahead. Facing pleural procedures can feel overwhelming, but you’re not facing this alone.
Pleural care teams can provide medical treatment alongside compassionate support. The procedures we’ve discussed – pleural biopsy and pleurodesis – have helped thousands of patients reclaim their health, their comfort, and their peace of mind.
Your courage in seeking information, asking questions, and advocating for your health demonstrates the strength that will carry you through this process. Successful pleural treatment outcomes depend not just on medical expertise, but on patients like you who are committed to their healing and willing to take positive steps forward.
The path to better breathing and improved quality of life begins with a single step – reaching out to a qualified pleural specialist who can evaluate your specific situation and recommend the best treatment approach for you. Don’t let fear or uncertainty delay the relief that could be within your reach.
If you’ve been advised to consider these procedures, speak with your thoracic specialist to discuss the best approach for your situation. You deserve expert care delivered with compassion, and that care is available to you right now. Your journey to healing, hope, and renewed health starts with that first phone call.
Remember: you are stronger than you know, braver than you feel, and more supported than you might realise. The medical community is here to help you through this challenge and guide you towards the relief and peace of mind you deserve.
Your better tomorrow begins today. Take that first step – you’ve got this, and we’re here to support you every step of the way.
FAQs
What is a pleural biopsy?
A pleural biopsy is a medical procedure where a small tissue sample is taken from the pleura, the membrane surrounding the lungs, to help diagnose conditions like infections or tumors.
Why would someone need a pleural biopsy?
Individuals may require a pleural biopsy to investigate the cause of pleural effusion, diagnose lung cancer, or assess other lung-related conditions.
Pleurodesis is a procedure that eliminates the pleural space to prevent fluid or air accumulation, often used in cases of recurrent pleural effusions.
Are there risks associated with pleural biopsy and pleurodesis?
Yes, both procedures carry risks, including bleeding, infection, and complications related to anesthesia. However, serious complications are relatively rare.
What benefits can I expect from undergoing pleurodesis?
Pleurodesis can provide significant relief from symptoms like breathlessness and reduce the need for frequent medical interventions related to fluid accumulation.