As a thoracic surgeon, you’re trained to expect high stakes. Every operation enters complex anatomical territory—vital structures, delicate tissues, unforgiving margins. But what training rarely prepares you for are the thoracic surgery complications themselves. They test your judgment, your team, and your resilience—and, if you’re willing to listen, they become your greatest teachers.
This post isn’t easy to write. But it’s important. These five complications were among the worst of my career—and each forced a critical evolution in how I practice, lead, and protect my patients.
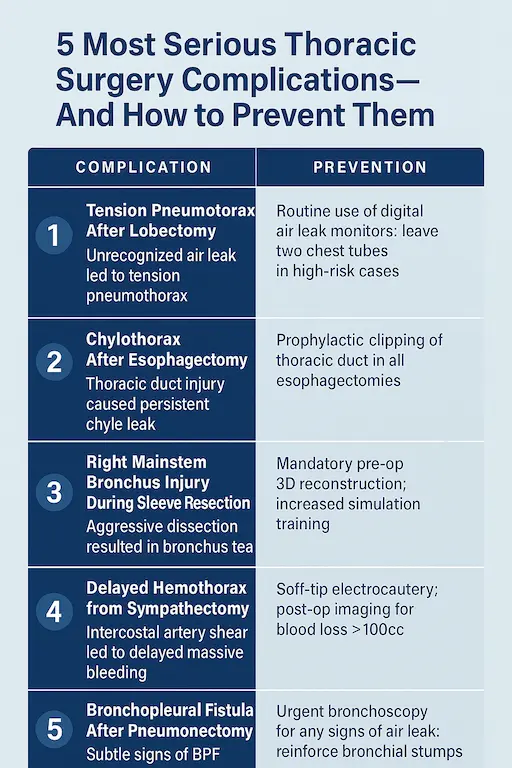
1. Tension Pneumothorax Post-Lobectomy — “We Didn’t See It Coming”
What happened: Within hours of a left upper lobectomy, the patient decompensated rapidly. This was a serious thoracic surgery complication: a tension pneumothorax from an unrecognized air leak caused mediastinal shift and hypotension.
Management: Immediate chest tube re-insertion and stabilization. Fortunately, the team responded fast.
What changed: We now use a digital air leak monitor post-op for all lobectomy patients. Nurses are trained to identify subtle changes in waveform early. We also leave a second chest tube in high-risk cases.
2. Chylothorax After Esophagectomy — “A Leak That Wouldn’t Stop”
What happened: A thoracic duct injury during an Ivor Lewis esophagectomy led to persistent high-output chyle leak. Despite conservative management, the patient developed malnutrition and needed reoperation.
Management: Surgical ligation of the thoracic duct on post-op day 10 resolved the issue.
What changed: We now routinely identify and prophylactically clip the thoracic duct in all esophagectomies. Additionally, early nutrition team involvement is mandatory for all high-output leaks past 72 hours.
3. Right Mainstem Bronchus Injury During Sleeve Resection — “Too Deep, Too Fast”
What happened: While performing a right upper lobe sleeve resection, an overly aggressive dissection near the carina resulted in a partial tear of the main bronchus.
Management: We repaired the injury intraoperatively, converted to open, and reinforced with intercostal muscle flap. The patient had prolonged ventilation and ICU stay but ultimately recovered.
What changed: All sleeve resections now involve mandatory pre-op 3D reconstruction for anatomical planning. We also increased simulation training for complex airway work and brought in a second attending for high-risk sleeves.
4. Delayed Massive Hemothorax from Intercostal Artery — “A Silent Bleed”
What happened: A minimally invasive sympathectomy went smoothly—until the patient returned 24 hours later in hemorrhagic shock. A sheared intercostal artery had retracted and clotted off initially, only to rebleed later.
Management: Emergent thoracotomy and artery ligation. The patient recovered but required transfusion and extended stay
What changed: We now use soft-tip electrocautery and avoid aggressive rib spreading in high-risk cases. Any blood loss over 100cc intra-op triggers 24-hour post-op imaging and observation, regardless of how “well” the case went.
5. Unrecognized Bronchopleural Fistula Post-Pneumonectomy — “A Whisper That Turned into a Storm”
What happened: A patient underwent a right pneumonectomy for central tumor. By day five, subtle subcutaneous emphysema appeared, but was initially attributed to benign causes. On day seven, the patient developed sepsis and was diagnosed with a bronchopleural fistula.
Management: The patient underwent Clagett window creation and long-term drainage. They eventually stabilized, but with significant morbidity.
What changed: Any post-pneumonectomy patient showing air leak signs—no matter how small—gets urgent bronchoscopy. We also started routinely reinforcing the bronchial stump with vascularized muscle or pericardium in high-risk patients.
Final Thoughts: Lessons Learned from Thoracic Surgery Complications
Most surgeons won’t admit this stuff publicly. But here’s the truth: the operating theatre humbles everyone. What defines us isn’t the absence of thoracic surgery complications—it’s how we respond to them.
Every one of these patients taught me something. Every mistake made me more careful, more systematic, and more collaborative.
To my colleagues: share your thoracic surgery complications. It’s how we all get better.
To patients: know that when a surgeon tells you “we’ve seen this before,” it often means we’ve lived the hard lesson—and changed because of it.