A collapsed lung can be frightening. Sudden chest pain, shortness of breath, and not knowing what to do can leave you anxious. This guide explains what a pneumothorax is, how it feels, what hospitals do, and when
minimally invasive surgery can prevent it from coming back. If you are in London and worried about symptoms, you can access rapid private assessment and same day investigations with Mr Marco Scarci, Consultant
Thoracic Surgeon.
What is a pneumothorax and who is at risk?
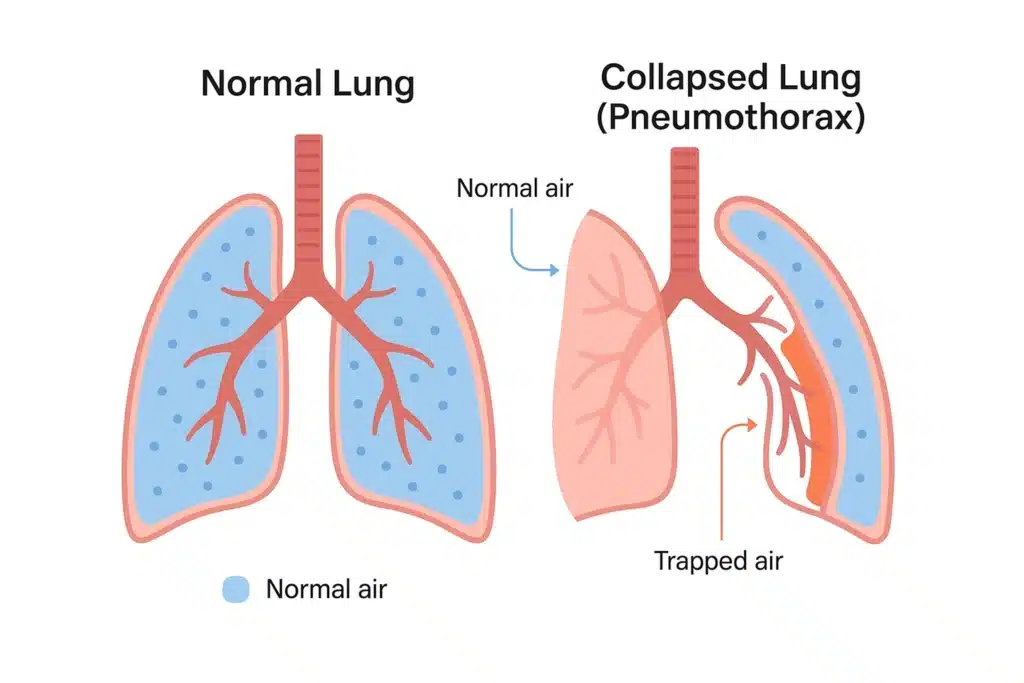
A pneumothorax happens when air leaks into the space around the lung, making it partially or completely collapse. There are three main types:
- Primary spontaneous pneumothorax, often in young, tall, slim people with no known lung disease, sometimes due to small blebs on the lung surface.
- Secondary spontaneous pneumothorax, in people with underlying lung problems such as COPD, asthma, cystic fibrosis, or previous infections, where symptoms are usually more severe.
- Traumatic or iatrogenic pneumothorax, after an injury, broken rib, medical procedure, or surgery.
You may have heard of the 2cm rule for pneumothorax. On a chest X ray, if the rim of air between the lung margin and chest wall is 2 cm or more, or if you have significant breathlessness, active treatment is usually advised rather than simple observation.
Those at highest risk include smokers, people with chronic lung disease, those with a family history of pneumothorax, and anyone who has already had one before.
How does a collapsed lung feel? Early warning signs
Typical pneumothorax signs and symptoms are:
- Sudden, sharp, one sided chest pain that may worsen with a deep breath or cough
- Breathlessness, from mild to severe
- Fast heart rate or feeling light headed
- A dry cough or tightness in the chest
Red flags that need urgent emergency care: severe breathlessness, fainting, blue lips or fingers, severe or increasing chest pain, coughing blood, or any rapid deterioration. Call 999 or go to A&E.
How it is diagnosed
In hospital, you will be examined and have a chest X ray. This usually confirms the diagnosis and the size of the pneumothorax. Learn more about symptoms and diagnosis on Patient.info. A CT scan may be used if the X ray is unclear, if there is suspicion of underlying lung disease, or when planning surgery. Oxygen levels and heart rhythm are monitored closely.
If you are uncertain whether your symptoms fit a pneumothorax, do not delay. Private rapid assessment can be arranged in London with same day imaging so you know exactly what is happening and what to do next. For more on symptoms and options, you can read our overview of pneumothorax treatment under pneumothorax signs and symptoms.
What does a hospital do for a collapsed lung?
Surgery is considered if:
- The lung does not fully re expand or keeps leaking air
- You have a recurrent pneumothorax, on the same or opposite side
- There is a high risk of recurrence due to blebs or underlying lung disease
- Your job or lifestyle makes recurrence particularly hazardous, for example pilots or divers
The modern approach is Video Assisted Thoracoscopic Surgery, also called VATS. Through two or three small incisions, your surgeon finds and treats the cause, often by removing fragile blebs or bullae and performing pleurodesis to help the lung adhere to the chest wall and reduce the chance of recurrence. Compared with open surgery, VATS usually means less pain, smaller scars, a shorter hospital stay, and a quicker return to normal activity, often within 2 to 4 weeks.
If you would like to understand these keyhole options, explore vats surgery and video-assisted thoracoscopic surgery for detail on how the procedure is performed and what to expect.
Pleurodesis, bleb resection, and prevention of recurrence
Pleurodesis creates a controlled inflammation that seals the pleural space so the lung stays expanded. It can be done surgically during VATS, sometimes combined with mechanical abrasion. Bleb resection, also called bullectomy when larger air sacs are involved, removes the weak areas that tend to burst. In experienced hands, this combined approach gives an excellent chance of preventing another collapse.
The definitive treatment for pneumothorax, when recurrence or persistent air leak is an issue, is surgical management with VATS bleb resection and pleurodesis. For first time, small, asymptomatic cases, conservative treatment remains appropriate.
Recovery timeline and what to avoid
After VATS, most patients:
- Spend one night in hospital, sometimes two
- Have a chest drain for about 24 hours
- Walk on the day of surgery, building activity gradually
- Return to desk work in 1 to 2 weeks, and to the gym by 3 to 4 weeks, if advised
What not to do after a pneumothorax:
- Do not fly until your specialist confirms that the pneumothorax has fully resolved on imaging
- Avoid scuba diving unless you have had definitive surgical treatment and have written clearance
- Do not lift heavy weights or strain for 1 to 2 weeks after conservative care, and for several weeks after surgery as advised
- Avoid smoking and vaping, since both increase the risk of recurrence
- Do not ignore new chest pain or breathlessness, even if mild, seek medical advice
Can you live a normal life after a pneumothorax? Yes. Most people return to full activity following appropriate treatment and recovery. If you undergo VATS with pleurodesis and bleb resection, the risk of another episode is significantly reduced, which helps you get back to life with confidence.
Private rapid access in London
Time matters with chest symptoms. Our practice offers rapid access consultations, often within an hour of first contact when appropriate, and can arrange same day chest X ray or CT. If you are already in a London hospital with a pneumothorax, we can provide prompt in hospital consultation and coordinate your care. We use minimally invasive techniques whenever suitable and tailor decisions through multidisciplinary discussion to give you the best chance of a smooth, fast recovery.
If you need a clear plan for prevention of recurrence, or simply want reassurance that you are healing well, we are here to help. You can also learn about pleurodesis on our pneumothorax treatment page for more detail about how we prevent a lung from collapsing again.

Summary
A collapsed lung is treatable, and in many cases it heals without surgery. The key is a precise diagnosis, a calm plan, and timely care. Small pneumothoraces can often be observed or treated with needle aspiration. Larger or
symptomatic cases may need a chest drain. If the problem comes back, or the air leak persists, VATS pleurodesis with bleb resection offers a minimally invasive, highly effective solution with less pain, shorter stay, and
faster return to normal life. If you are in London and worried about symptoms now, seek urgent care for red flags and contact our private clinic for rapid assessment and a personalised treatment plan.