
Empyema is a serious condition that can cause chest pain, breathlessness, and fatigue. Maria clutched her chest as another wave of pain shot through her ribs. What had started as a simple cold three weeks ago had transformed into something far more sinister. Her GP had initially prescribed antibiotics, but now, sitting in the chest physician’s office, she was hearing words that made her heart race: “empyema,” “surgical intervention,” and “thoracic surgery.” Like thousands of patients each year, Maria was about to embark on a journey that would test her resilience but ultimately restore her ability to breathe freely again.
The Silent Threat: Understanding Empyema
Empyema, a severe chest infection characterised by the accumulation of infected fluid in the pleural space surrounding the lungs, affects approximately 65,000 individuals annually. This condition transforms the normally smooth, lubricated cavity between the lung and chest wall into a battlefield where infection wages war against the body’s natural healing mechanisms.
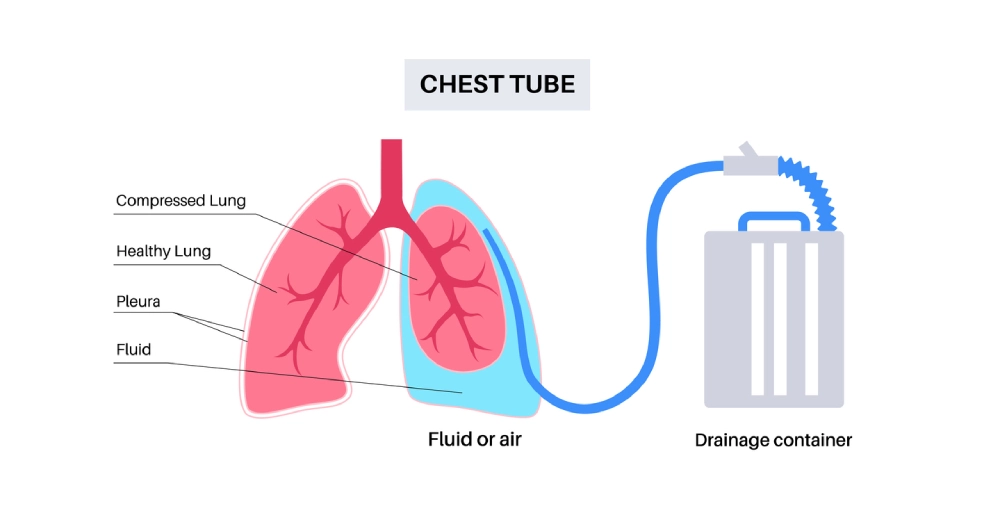
What makes empyema particularly challenging is its progressive nature. Unlike simple pneumonia that primarily affects lung tissue, empyema involves the pleural cavity—the delicate space that allows our lungs to expand and contract with each breath. When infection invades this space, it can create thick, infected fluid collections (we call them effusions) that compress the lung, making breathing increasingly difficult and potentially life-threatening.
The Three Stages of Empyema Development
Most of the time, a pleural infection is the consequence of a parapneumonic effusion, which means that pneumonia could expand in the lung tissue, causing a lung abscess and also irritate the lining of the chest wall, causing a pleural effusion (we call it complicated parapneumonic effusion), and a pleural space infection other times it could be the result of chest trauma. Medical professionals classify empyema into three distinct stages, each requiring increasingly aggressive treatment approaches:
- Stage 1 (Exudative Phase): In the earliest stage, thin, infected fluid begins accumulating in the pleural space. At this point, minimally invasive procedures like thoracentesis or chest tube drainage may effectively resolve the infection together with long-term antibiotic therapy. Patients often experience chest pain, fever, and shortness of breath, but the condition remains highly treatable with prompt medical intervention.
- Stage 2 (Fibrinopurulent Phase): As the infection progresses, the pleural fluid becomes thick and fibrous, containing white blood cells, bacteria, and cellular debris. A simple chest drain becomes less effective as the infected material takes on a consistency similar to thick honey. This stage typically occurs 7-21 days after initial infection and often requires more sophisticated surgical drainage procedures or intrapleural fibrinolytic therapy. This is the injection into the infected pleural space of fibrinolytic agents, which are like solvents that aim to melt the thick material inside the chest that forms the pleural empyema. That drug is called tissue plasminogen activator (TPA for short).
- Stage 3 (Organising Phase): The most advanced stage involves the formation of a thick, fibrous “peel” or cortex around the lung. This rigid shell can permanently restrict lung expansion, leading to chronic breathing problems and reduced quality of life. Advanced thoracic surgery becomes necessary to remove this constraining layer and restore normal lung function and movement of the thoracic cavity. Surgery is normally reserved when intrapleural fibrinolytic therapy fails with ongoing sepsis and persistent thoracic empyema.
When Surgery Becomes Essential: Recognising the Need for Intervention
Mr Marco Scarci, a renowned thoracic surgeon at a leading medical center, explains the decision-making process: “When I meet patients like Maria, I see not just the medical complexity of their condition, but the human story behind it. Every case of empyema, especially with bronchopleural fistula, represents someone’s struggle to breathe, to return to their family, to regain their independence.”
Clinical Indicators for Surgical Treatment
Surgical intervention for empyema becomes necessary when several factors align:
- Failed Conservative Treatment: When antibiotics and simple chest tube drainage fail to resolve the infection, surgical options must be considered. Studies show that delayed surgical intervention can lead to prolonged hospital stays, increased complications, and higher healthcare costs.
- Complex Fluid Collections: Advanced imaging techniques, such as CT scans, may reveal multiple, loculated (compartmentalised) fluid collections that cannot be adequately drained through simple tube placement in complex empyema thoracis. These complex collections require surgical access to ensure complete evacuation.
- Significant Lung Compression: When the infected fluid collection compresses more than 30% of the lung volume, breathing becomes severely compromised. Emergency surgical drainage may be required to prevent respiratory failure.
- Pleural Disease Septic Complications: Patients showing signs of systemic infection and sepsis, including high fever, elevated white blood cell count, and organ dysfunction, may require urgent surgical intervention to control the source of infection.
The Human Cost of Delayed Treatment
James, a 52-year-old construction worker, initially tried to “tough out” his chest symptoms, believing they would resolve on their own. “I thought it was just a bad chest cold,” he recalls. “But when I couldn’t climb a flight of stairs without gasping for air, I knew something was seriously wrong.” His delayed presentation resulted in Stage 3 empyema, requiring extensive surgical intervention that could have been avoided with earlier treatment.
Surgical Treatment Options: From Minimally Invasive to Complex Procedures
Modern thoracic surgery offers a spectrum of treatment options, each tailored to the specific stage and complexity of the empyema. Board-certified thoracic surgeons work closely with pulmonologists, infectious disease specialists, and critical care teams to determine the most appropriate surgical approach.
Video-Assisted Thoracoscopic Surgery (VATS)
VATS has become an important advancement in thoracic surgery, offering patients a minimally invasive alternative to traditional open surgery. This technique uses small incisions (typically 1-2 centimeters) and a tiny camera to guide surgical instruments within the chest cavity.
Benefits of VATS include:
- Reduced postoperative pain
- Shorter hospital stays
- Faster recovery times
- Improved cosmetic outcomes
- Lower risk of complications
Mr Marco Scarci, who has performed over 500 of those VATS procedures and is the first author of the European guidelines for the treatment of empyema, explains: “When I can offer a patient like Maria a minimally invasive option, I see the relief in their eyes. They understand that their path to recovery will be gentler, with less pain and a quicker return to their normal activities.”
The VATS procedure typically involves:
- Patient positioning under general anaesthesia
- Small incision placement for the camera and instruments
- Thoracoscopic visualisation of the pleural cavity
- Infected fluid evacuation and debridement
- Pleural space irrigation with an antibiotic solution
- Chest tube placement for continued drainage
Open Thoracotomy: When Extensive Surgery is Required
For advanced Stage 3 empyema or cases with significant complications, open thoracotomy may be necessary. While more invasive than VATS, this approach provides surgeons with complete access to the pleural cavity, allowing for comprehensive treatment of complex infections.
Decortication procedures through open thoracotomy involve:
- Extensive surgical exposure through a larger chest incision
- Complete removal of the fibrous peel surrounding the lung
- Lung re-expansion to restore normal breathing capacity
- Comprehensive debridement of all infected tissue
Emerging Techniques: Robotic-Assisted Surgery
Robotic thoracic surgery is increasingly being utilised for complex empyema cases, combining the precision of robotic technology with the benefits of minimally invasive techniques. This approach offers enhanced visualisation and improved dexterity for intricate surgical maneuvers.
The Surgical Journey: What Patients Can Expect
Understanding the surgical process helps patients and families prepare for the journey ahead. Experienced medical teams guide patients through each step, ensuring comprehensive care and support.
Preoperative Preparation
Comprehensive preoperative evaluation includes:
- Detailed medical history and physical examination
- Advanced imaging studies (CT scans, possibly MRI)
- Pulmonary function tests to assess breathing capacity
- Cardiac evaluation to ensure surgical safety
- Laboratory studies, including blood work and cultures
- Anaesthesia consultation for perioperative planning
The Surgical Experience
Sarah, who underwent VATS for Stage 2 empyema, describes her experience: “The medical team explained everything beforehand, which really helped with my anxiety. When I woke up after surgery, I could already breathe easier. The chest tube was uncomfortable, but knowing it was helping drain the infection made it bearable.”
Typical surgical timeline:
- Procedure duration: 1-4 hours, depending on complexity
- Anaesthesia recovery: 1-2 hours in post-anaesthesia care
- Initial monitoring: 24-48 hours in intensive care or step-down unit
- Chest tube management: 3-7 days average duration
- Hospital stay: 5-10 days for uncomplicated cases
Postoperative Recovery and Pain Management
Comprehensive pain management protocols ensure patient comfort during recovery:
- Multimodal analgesia combining different pain-relief methods
- Epidural anaesthesia for major procedures
- Patient-controlled analgesia (PCA) pumps
- Regional nerve blocks for targeted pain relief
- Non-pharmacological approaches, including positioning and breathing exercises
Complications and Risk Management
While surgical treatment of empyema is generally safe and effective, understanding potential complications helps patients make informed decisions about their care.
Common Postoperative Challenges
Air leaks occur in 15-20% of patients but typically resolve within a few days with chest tube management. Bleeding requiring intervention is rare (less than 2% of cases) but necessitates immediate medical attention. Infection recurrence affects approximately 5-10% of patients, particularly those with underlying health conditions or compromised immune systems.
Long-term Considerations
Pulmonary function recovery varies among patients, with most experiencing significant improvement within 3 to 6 months. Physical rehabilitation plays a crucial role in optimising outcomes, with structured pulmonary rehabilitation programs showing excellent results.
Dr. Lisa Wang, a pulmonary rehabilitation specialist, notes: “Patients who actively participate in breathing exercises and gradual activity progression often exceed their pre-illness functional capacity. The human body’s ability to heal and adapt is remarkable when given the proper support.”
Choosing the Right Medical Team

Selecting experienced healthcare providers has a significant impact on treatment outcomes. Patients should seek medical centers with:
Specialised Expertise
- Thoracic surgeons with extensive empyema experience
- Multidisciplinary teams, including pulmonologists, infectious disease specialists, and critical care physicians
- Advanced surgical facilities equipped with modern thoracoscopic and robotic technology
- Comprehensive support services, including respiratory therapy and rehabilitation programs
Quality Metrics and Outcomes
Experienced thoracic surgery programs typically demonstrate:
- Low complication rates compared to national benchmarks
- Shorter average hospital stays indicate efficient care
- High patient satisfaction scores reflecting quality service
- Robust infection control protocols ensure patient safety
Insurance Coverage and Financial Considerations
Insurance coverage for empyema surgery varies depending on the specific procedure and insurance plan. Most insurance providers, including Medicare and Medicaid, recognise surgical treatment of empyema as medically necessary when conservative treatment has failed.
Understanding Healthcare Costs
Surgical treatment costs can vary significantly based on:
- Procedure complexity (VATS vs. open surgery)
- Hospital length of stay
- Geographic location of the medical facility
- Surgeon and facility experience levels
- Postoperative complications requiring additional treatment
Most hospitals have staff who can help patients review insurance coverage and discuss payment options if needed.
Life After Surgery: Recovery and Beyond
The journey doesn’t end when patients leave the hospital. Long-term recovery from empyema surgery involves multiple phases, each with its own milestones and challenges.
The First Month: Foundation for Healing
During the initial weeks following surgery, patients focus on:
- Wound care and monitoring for signs of infection
- Gradual activity progression under medical supervision
- Breathing exercises to promote lung re-expansion
- Pain management with decreasing medication requirements
- Follow-up appointments to assess healing progress
Months 2-6: Building Strength and Endurance
As healing progresses, patients typically experience:
- Increased exercise tolerance and stamina
- Return to routine activities, including work and hobbies
- Improved breathing capacity approaching normal levels
- Psychological adjustment to their recovery journey
- Ongoing medical monitoring to prevent complications
Long-term Outlook: Returning to Full Life
Thomas, now two years post-surgery, reflects on his journey: “I never thought I’d be grateful for something as simple as taking a deep breath. The surgery gave me my life back. I’m hiking again, playing with my grandchildren, and sleeping through the night without coughing.”
Research shows that most patients achieve:
- 85-95% restoration of pre-illness lung function
- Significant improvement in quality of life measures
- Low recurrence rates (less than 5% with appropriate follow-up)
- Return to baseline activity levels within 6-12 months
Prevention and Future Considerations
While not all cases of empyema can be prevented, understanding risk factors and maintaining good health practices can reduce the likelihood of developing this serious condition.
Risk Reduction Strategies
Preventive measures include:
- Prompt treatment of respiratory infections
- Vaccination against pneumonia and influenza
- Smoking cessation to improve lung health
- Regular medical care for chronic conditions
- Maintaining strong immune function through healthy lifestyle choices
Advances in Treatment
Emerging therapies continue to improve outcomes for empyema patients:
- Enhanced imaging techniques for better surgical planning
- Improved antibiotics targeting resistant organisms
- Advanced drainage systems for more effective fluid removal
- Biomarker research for earlier diagnosis
- Minimally invasive innovations reducing surgical trauma
Finding Hope in Healing

The diagnosis of empyema can feel overwhelming, but advances in surgical treatment offer hope and healing to thousands of patients each year. Expert medical teams across the country are equipped with the knowledge, technology, and compassion necessary to guide patients through this challenging journey.
Maria, whose story began this article, successfully underwent VATS surgery and returned to her active lifestyle within three months. “The hardest part was the fear of the unknown,” she shares. “But my surgical team explained everything, answered all my questions, and supported me every step of the way. Today, I breathe freely and appreciate every moment.”
Taking the Next Step
If you or a loved one is facing a diagnosis of empyema, remember that timely surgical intervention can dramatically improve outcomes and quality of life. Consulting with experienced thoracic surgeons and understanding all available treatment options empowers patients to make informed decisions about their care.
Leading medical centers offer comprehensive consultations where patients can:
- Meet with surgical specialists to discuss treatment options
- Receive second opinions on recommended procedures
- Tour surgical facilities and meet care team members
- Access patient resources and support services
- Connect with other patients who have undergone similar procedures
Recovering from empyema takes time, but with the right treatment and support, most patients regain normal breathing and strength.
In the battle against severe chest infection, patients are not alone. Dedicated healthcare teams stand ready to provide the expertise, technology, and support necessary to guide each person through their unique healing journey, from diagnosis to full recovery and beyond.