Introduction: When Breathing Becomes a Monthly Challenge
For women experiencing catamenial pneumothorax, each menstrual cycle can bring unexpected respiratory distress that disrupts daily life and creates significant anxiety. This rare but serious condition affects approximately 3-6% of women with spontaneous pneumothorax, yet it remains underdiagnosed and often misunderstood. Understanding the available treatment options, from conservative management to advanced surgical interventions, is crucial for both patients and healthcare providers navigating this complex condition.
Catamenial pneumothorax represents a unique intersection of gynecological and pulmonary medicine, requiring specialised knowledge and a multidisciplinary approach to achieve optimal outcomes. While diagnosis and treatment can take time, most patients experience significant improvement with appropriate medical and surgical care.
Understanding Catamenial Pneumothorax: The Medical Foundation
What Makes This Condition Unique
Catamenial pneumothorax is a rare form of spontaneous pneumothorax that occurs cyclically in conjunction with menstruation, typically within 72 hours of menstrual onset. The term “catamenial” derives from the Greek word “katamenia,” meaning monthly discharge, highlighting the condition’s distinctive temporal relationship with the menstrual cycle.
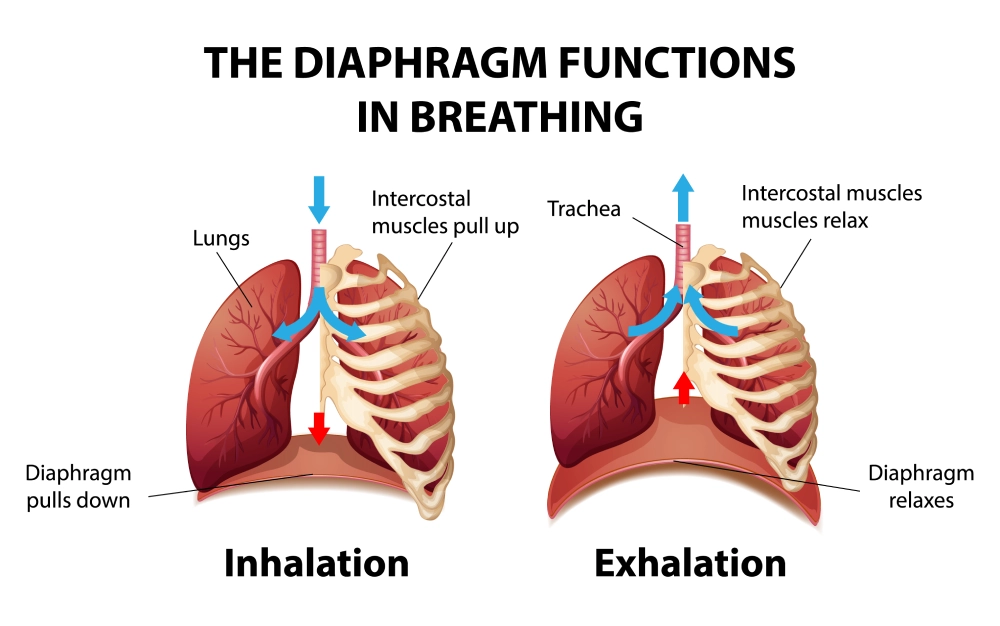
This condition primarily affects women of reproductive age, with peak incidence occurring between the ages of 20-40. The underlying pathophysiology involves thoracic endometriosis, where endometrial tissue or endometrial stroma implants on the pleura or diaphragm, creating cyclical inflammation and visceral pleura (the lining of the lung) breakdown that can lead to air leakage into the pleural space. Migration into the chest is thought to be caused by diaphragmatic fenestration or larger diaphragmatic defects that allow movement of endometrial cells from the peritoneal cavity to the thoracic cavity. This condition is called thoracic endometriosis syndrome or pleural endometriosis.
Clinical Presentation and Symptoms
Women with catamenial pneumothorax (lung collapse) typically present with:
- Acute chest pain: Often described as sharp, stabbing pain that may radiate to the shoulder
- Shortness of breath: Ranging from mild dyspnea to severe respiratory distress
- Cyclical pattern: Symptoms occurring within 24-72 hours of menses
- Right-sided predominance: Approximately 90% of cases affect the right lung
- Recurrent episodes: Without proper treatment, episodes tend to recur with subsequent menstrual cycles
The diagnostic challenge lies in recognising the pattern, as many patients and healthcare providers may not initially connect respiratory symptoms with menstruation. This delay in recognition can lead to repeated emergency department visits and inappropriate treatments. Usually, those patients have a history of chest tube placement in A&E before someone realises the connection with endometriosis.
Comprehensive Treatment Approaches
Conservative Medical Management
Hormonal Therapy: First-Line Treatment Options
Continuous Oral Contraceptives: For many women with catamenial pneumothorax, continuous oral contraceptive therapy represents an effective first-line treatment. By suppressing ovulation and eliminating menstrual cycles, hormonal contraceptives can significantly reduce or eliminate pneumothorax recurrence.
Benefits include:
- Non-invasive treatment approach
- Cost-effective long-term management
- Additional benefits for menstrual-related symptoms
- Reversible intervention allowing future fertility

GnRH Agonists: Advanced Hormonal Suppression Gonadotropin-releasing hormone (GnRH) agonists such as leuprolide or goserelin provide more complete hormonal suppression for severe cases. These medications create a temporary menopausal state, effectively eliminating the hormonal fluctuations that trigger endometrial tissue activity.
Treatment considerations:
- Typically prescribed for 6-12 months
- Requires careful monitoring for menopausal side effects
- May include add-back hormone therapy to minimise bone loss
- Excellent efficacy rates for pneumothorax prevention
Danazol: Alternative Hormonal Approach Danazol, an androgenic steroid, offers another hormonal treatment option with unique benefits for endometriosis management. This medication suppresses both estrogen and progesterone production while providing mild androgenic effects.
Clinical advantages:
- Direct anti-endometrial effects
- Lower cost compared to GnRH agonists
- Fewer menopausal side effects
- Effective for concurrent pelvic endometriosis
Surgical Treatment Options
Video-Assisted Thoracoscopic Surgery (VATS)
The Gold Standard for Surgical Management: Video-assisted thoracoscopic surgery has emerged as the preferred surgical approach for catamenial pneumothorax treatment. This minimally invasive technique allows thoracic surgeons to directly visualise and treat endometrial implants while addressing associated pleural abnormalities.
VATS procedure benefits:
- Minimal chest wall trauma
- Reduced postoperative pain
- Shorter hospital stays
- Excellent cosmetic outcomes
- Comprehensive treatment of underlying pathology
Surgical Techniques and Procedures
During VATS for catamenial pneumothorax, surgeons typically perform several key interventions:
- Thorough pleural inspection: Systematic examination of all pleural surfaces to identify endometrial implants
- Diaphragmatic repair: Treatment of diaphragmatic perforations or thinning
- Pleurodesis: Mechanical or chemical pleurodesis to prevent recurrence
- Bullae management: Resection of pulmonary blebs or bullae when present
Diaphragmatic Surgery: Addressing the Root Cause
Plication and Repair: Many cases of catamenial pneumothorax involve diaphragmatic abnormalities, including perforations, thinning, or endometrial implants. Surgical repair of these defects is crucial for long-term success and is better addressed by going through the chest cavity.
Surgical approaches include:
- Primary repair: Direct suturing of small perforations
- Plication: Reinforcement of thinned diaphragmatic areas
- Patch repair: Use of synthetic or biological materials for larger defects
- Complete diaphragmatic resection: Reserved for extensive disease
Pleurodesis: Preventing Future Episodes
Mechanical Pleurodesis Techniques: Mechanical pleurodesis involves creating adhesions between the visceral and parietal pleura to eliminate the pleural space and prevent future pneumothorax episodes.
Common techniques:
- Pleural abrasion: Mechanical scarring of pleural surfaces
- Parietal pleurectomy: Removal of parietal pleural tissue
- Electrocautery pleurodesis: Using electrical energy to create adhesions
Chemical Pleurodesis Options: Chemical agents can also create effective pleural adhesions:
- Talc pleurodesis: Most commonly used and highly effective
- Tetracycline derivatives: An Alternative for patients with talc allergies
- Autologous blood patch: Natural option with success rates
Multidisciplinary Care Coordination

The Importance of Integrated Treatment Teams
Successful management of catamenial pneumothorax requires coordination between multiple medical specialties:
Pulmonology Specialists
- Initial diagnosis and acute management
- Long-term respiratory monitoring
- Coordination of treatment protocols
- Patient education and support
Gynecology and Reproductive Endocrinology
- Hormonal therapy management
- Treatment of concurrent pelvic endometriosis
- Fertility counseling and planning
- Long-term reproductive health monitoring
Thoracic Surgery
- Surgical intervention planning
- Minimally invasive surgical techniques
- Postoperative care management
- Long-term surgical follow-up
Advanced Treatment Strategies
Emerging Therapeutic Options
Targeted Hormonal Therapies
Aromatase Inhibitors: Recent research has explored the use of aromatase inhibitors such as letrozole for catamenial pneumothorax management. These medications block local estrogen production in endometrial tissue, offering a targeted approach to treatment.
Potential benefits:
- Specific action on endometrial tissue
- Fewer systemic hormonal effects
- Effective for hormone-resistant cases
- Preservation of reproductive function
Selective Estrogen Receptor Modulators (SERMs): SERMs like raloxifene provide tissue-specific estrogen receptor activity, potentially offering benefits for catamenial pneumothorax while maintaining bone health and cardiovascular protection.
Novel Surgical Techniques
Robotic-Assisted Surgery: Providing improved visualisation and precision for complex procedures.
Advantages include:
- Superior dexterity and precision
- Enhanced visualisation of small implants
- Reduced surgeon fatigue
- Potential for better long-term outcomes
Hybrid Approaches: Combining surgical and medical therapies can optimise treatment outcomes:
- Surgical treatment followed by hormonal suppression
- Preoperative hormonal therapy to reduce implant activity
- Postoperative hormonal maintenance therapy
Managing Treatment Complications
Surgical Complications and Management
Immediate Postoperative Concerns
- Air leaks: Monitoring and management of persistent air leaks
- Pain management: Multimodal approaches to minimise discomfort
- Infection prevention: Appropriate antibiotic protocols
- Respiratory monitoring: Ensuring adequate pulmonary function
Long-term Follow-up Considerations
- Recurrence surveillance: Regular imaging and clinical assessment
- Pleural adhesion monitoring: Evaluation of pleurodesis effectiveness
- Functional outcome assessment: Pulmonary function testing and quality of life measures
Hormonal Therapy Side Effects
Managing Menopausal Symptoms: For patients receiving GnRH agonist therapy:
- Hot flash management: Lifestyle modifications and targeted therapies
- Bone health protection: Calcium, vitamin D, and bone density monitoring
- Cardiovascular risk assessment: Lipid monitoring and lifestyle counseling
- Mood and cognitive support: Psychological support and intervention
Patient-Centered Care Approaches
Quality of Life Considerations
Physical Health Optimisation
Living with catamenial pneumothorax extends beyond managing the immediate respiratory symptoms. Patients require comprehensive support to maintain optimal physical health throughout their treatment journey.
Pulmonary Rehabilitation Programs: Specialised pulmonary rehabilitation can help patients:
- Improve respiratory muscle strength
- Develop effective breathing techniques
- Enhance overall exercise tolerance
- Build confidence in physical activities
Nutritional Support: Proper nutrition supports healing and overall health:
- Anti-inflammatory dietary approaches
- Adequate protein for tissue repair
- Calcium and vitamin D for bone health during hormonal therapy
- Nutritional counseling for optimal recovery
Psychological and Emotional Support
Anxiety and Depression Management: The unpredictable nature of catamenial pneumothorax can create significant psychological distress. Comprehensive care includes:
- Cognitive behavioural therapy: Developing coping strategies for anxiety
- Support groups: Connecting with others who understand the condition
- Stress management techniques: Mindfulness, relaxation, and stress reduction
- Professional counseling: Addressing depression and anxiety disorders
Fertility and Family Planning Concerns: Many treatment options affect reproductive function, requiring sensitive counseling:
- Fertility preservation options: Before starting hormonal suppression
- Family planning discussions: Timing pregnancies around treatment
- Contraceptive counseling: Safe options for sexually active patients
- Reproductive endocrinology consultation: Specialised fertility support
Long-Term Management Strategies
Monitoring and Surveillance Programs
Regular Follow-up Protocols: Successful long-term management requires systematic monitoring:
- Clinical assessments: Regular symptom evaluation and physical examination
- Imaging surveillance: Chest X-rays or CT scans as appropriate
- Pulmonary function testing: Monitoring respiratory capacity and function
- Hormonal level monitoring: For patients receiving hormonal therapy
Patient Education and Self-Management: Empowering patients with knowledge and skills:
- Symptom recognition: Early identification of pneumothorax recurrence
- Emergency action plans: When and how to seek immediate medical attention
- Medication management: Proper use of hormonal therapies
- Lifestyle modifications: Activities and precautions to reduce risk
Individualised Treatment Plans
Personalised Medicine Approaches: Treatment plans must consider individual patient factors:
- Age and reproductive goals: Balancing treatment efficacy with fertility preservation
- Severity and frequency: Matching treatment intensity to disease severity
- Comorbid conditions: Considering other health conditions in treatment selection
- Patient preferences: Incorporating patient values and treatment preferences
Adaptive Treatment Strategies: Treatment plans should evolve based on:
- Response to initial therapy: Adjusting approaches based on effectiveness
- Side effect profiles: Modifying treatments to minimise adverse effects
- Life stage changes: Adapting to pregnancy, menopause, and ageing
- New therapeutic options: Incorporating advances in medical knowledge
Future Directions and Research
Emerging Treatment Modalities
Genetic and Molecular Therapies
Research into the genetic and molecular basis of endometriosis is opening new therapeutic possibilities:
Targeted Molecular Therapies
- Anti-angiogenic agents: Targeting blood vessel formation in endometrial implants
- Inflammatory pathway inhibitors: Blocking specific inflammatory cascades
- Growth factor antagonists: Preventing endometrial tissue growth and invasion
Genetic Testing and Personalised Medicine
- Biomarker identification: Developing tests to predict treatment response
- Pharmacogenomics: Tailoring medications to individual genetic profiles
- Risk stratification: Identifying patients at highest risk for recurrence
Technological Advances
Advanced Imaging Techniques
- High-resolution CT protocols: Better detection of small endometrial implants
- MRI innovations: Enhanced soft tissue characterisation
- PET imaging: Metabolic assessment of endometrial tissue activity
Minimally Invasive Technologies
- Flexible thoracoscopy: Expanded diagnostic and therapeutic capabilities
- Electromagnetic navigation: Improved localisation of lung lesions
- Advanced energy devices: Better tissue sealing and cutting technologies
Research Priorities and Clinical Trials
Current Research Focus Areas
Hormonal Therapy Optimisation: Ongoing studies examine:
- Optimal duration of hormonal suppression
- Combination hormonal therapies
- Novel hormonal delivery systems
- Selective tissue targeting approaches
Surgical Technique Refinement: Research efforts include:
- Comparative effectiveness studies: Evaluating different surgical approaches
- Long-term outcome assessment: Following patients for extended periods
- Quality of life measures: Assessing patient-reported outcomes
- Cost-effectiveness analysis: Determining optimal resource allocation
Future Clinical Trial Opportunities
Patients with catamenial pneumothorax may benefit from participation in clinical trials investigating:
- New hormonal suppression agents
- Novel surgical techniques
- Combination therapy approaches
- Biomarker-guided treatment selection
Cost Considerations and Healthcare Economics
Economic Impact of Treatment Options
Direct Medical Costs
Conservative Management Expenses
- Hormonal therapy costs: Monthly medication expenses and monitoring
- Regular follow-up visits: Ongoing healthcare provider consultations
- Imaging studies: Periodic chest imaging and surveillance
- Laboratory monitoring: Hormone levels and safety assessments
Surgical Intervention Costs
- Hospital stay expenses: Operating room time and recovery costs
- Surgeon fees: Specialist consultation and procedure costs
- Anaesthesia costs: Professional fees and medication expenses
- Postoperative care: Follow-up visits and complication management
Indirect Economic Considerations
Quality-Adjusted Life Years (QALYs): Economic analyses increasingly consider:
- Symptom-free time: Value of periods without pneumothorax episodes
- Functional capacity: Ability to work and perform daily activities
- Long-term health outcomes: Prevention of chronic complications
- Patient satisfaction: Quality of life improvements
Productivity and Work Impact
- Reduced sick leave: Fewer work absences due to acute episodes
- Improved work performance: Better concentration and physical capacity
- Career advancement: Reduced impact on professional development
- Healthcare utilisation: Decreased emergency department visits
Insurance Coverage and Access
Coverage Considerations
Prior Authorisation Requirements: Many insurance plans require:
- Documentation of diagnosis: Proper coding and clinical evidence
- Treatment history: Evidence of conservative management attempts
- Specialist consultation: Confirmation from appropriate specialists
- Cost-benefit analysis: Justification for expensive interventions
Appeal Processes: When coverage is denied:
- Medical necessity appeals: Providing additional clinical documentation
- Peer-to-peer reviews: Direct physician communication with insurers
- External review options: Independent medical review processes
- Patient advocacy: Support from the healthcare team and patient organisations
Conclusion: Hope and Healing for the Future

Treatment options continue to evolve, improving outcomes for women affected by this condition. From conservative hormonal management to advanced surgical techniques, the array of available treatments allows for individualised approaches that can effectively control symptoms while preserving quality of life and reproductive health.
The key to successful treatment lies in early recognition, proper diagnosis, and the development of a comprehensive treatment plan that addresses both the immediate respiratory concerns and the underlying endometrial pathology. Through collaboration between patients and their healthcare teams, including pulmonologists, gynecologists, and thoracic surgeons, optimal outcomes can be achieved.
As research continues to advance our understanding of catamenial pneumothorax, new therapeutic options will undoubtedly emerge. Ongoing research aims to develop more effective and less invasive treatment options.
For women currently living with catamenial pneumothorax, the message is clear: effective treatments exist, and with proper medical care, it is possible to regain control over respiratory health and return to a full, active life. Although treatment can be complex, most patients recover well with proper care and follow-up.
The medical community’s growing awareness and expertise in managing this condition, combined with ongoing research efforts and technological advances, ensures that the prognosis for women with catamenial pneumothorax continues to improve. Through continued advocacy, education, and research, we can work together to ensure that all women affected by this condition have access to the comprehensive care they need and deserve.