Understanding your treatment options when breathing becomes a daily challenge
Introduction: You’re Not Alone in This Journey
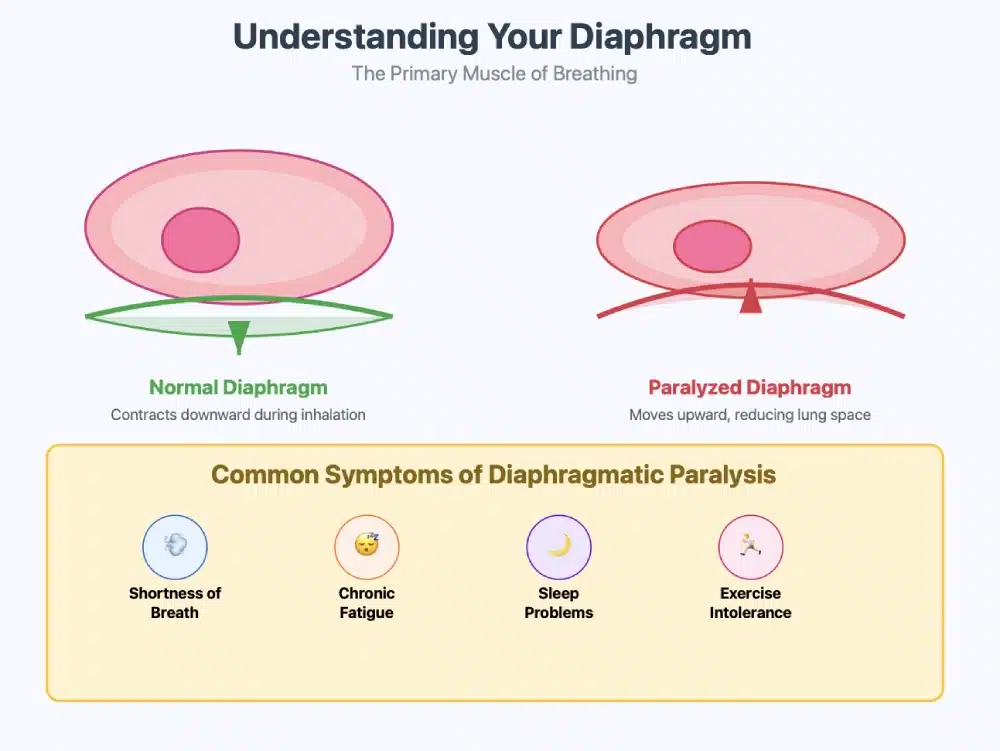
If you’re reading this, you or someone you love may be facing the frightening reality of diaphragmatic paralysis or eventration. The shortness of breath, the fatigue, the worry about what comes next – these feelings are completely understandable. What you’re experiencing is real, and more importantly, there is hope.
Diaphragmatic plication is a proven surgical procedure that has helped thousands of patients reclaim their breath and their lives. This comprehensive guide will walk you through everything you need to know about this life-changing treatment, from understanding your condition to recovery and beyond.
Understanding Your Diaphragm: The Unsung Hero of Breathing
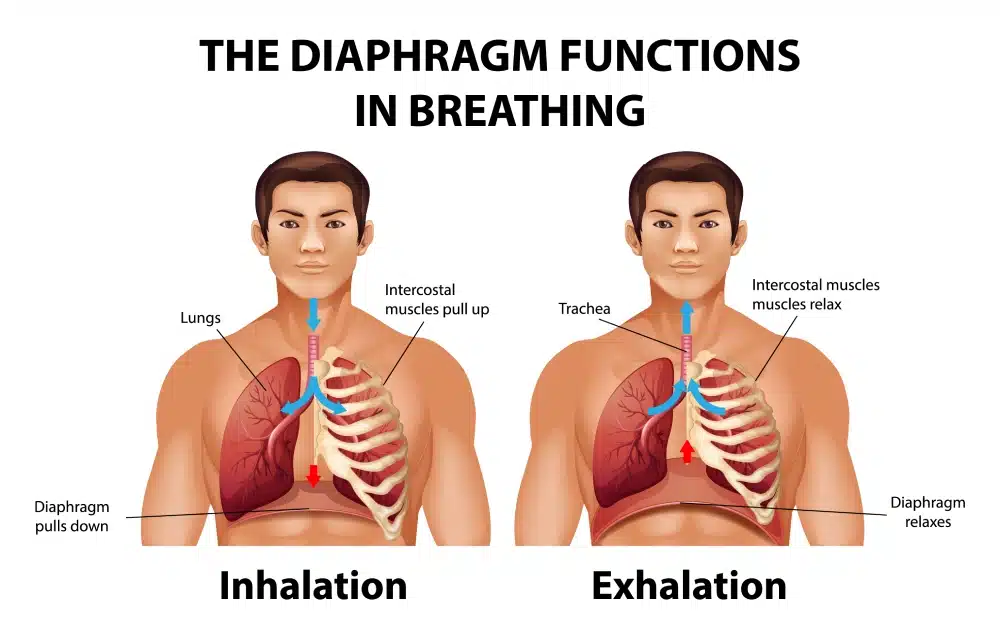
Your diaphragm is a dome-shaped muscle that sits beneath your lungs, acting as the primary driver of your breathing. When healthy, it contracts and flattens during inhalation, creating space for your lungs to expand. During exhalation, it relaxes and returns to its dome shape, helping push air out of your lungs.
When your diaphragm becomes paralysed or weakened (a condition called diaphragmatic paralysis, sometimes referred to as eventration), this natural rhythm is disrupted. Instead of moving down as it should, part of the diaphragm moves upward, working against your breathing. This creates the exhausting cycle of breathlessness that many patients describe as “feeling like I’m drowning in air.”
What Is Diaphragmatic Plication?
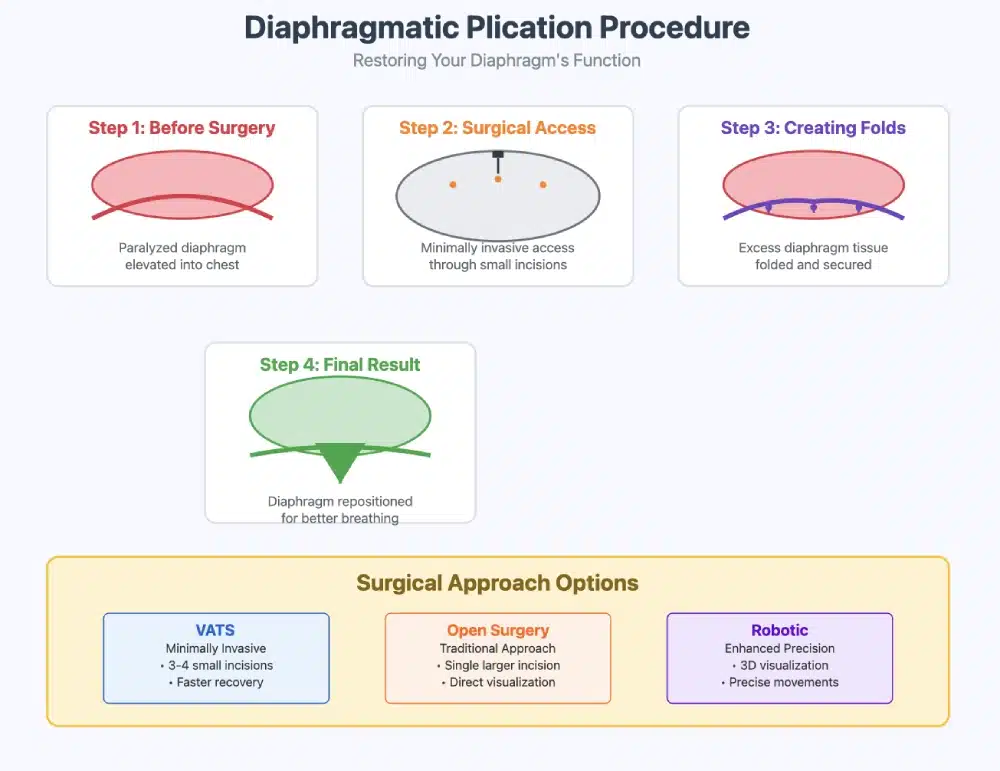
Diaphragmatic plication is a surgical procedure designed to restore the normal position and function of your diaphragm. The word “plication” comes from the Latin word meaning “to fold.” During this procedure, your surgeon carefully folds and secures the weakened or paralysed portion of your diaphragm, creating a tighter, more stable surface that can better support your breathing.
Think of it like tailoring a loose garment – by taking in the excess material and securing it in place, the surgeon creates a more functional structure that works in harmony with your healthy lung tissue.
Types of Diaphragmatic Conditions Treated
- Diaphragmatic Paralysis: This occurs when the phrenic nerve, which controls your diaphragm, is damaged or cut. This can happen during heart surgery, lung surgery, or due to trauma, infection, or tumors.
- Diaphragmatic Eventration: This is a condition where the diaphragm muscle itself is weakened or underdeveloped, causing it to balloon upward into the chest cavity.
- Unilateral vs. Bilateral: The condition can affect one side (unilateral) or both sides (bilateral) of your diaphragm. Unilateral cases are more common and often have better outcomes with plication.
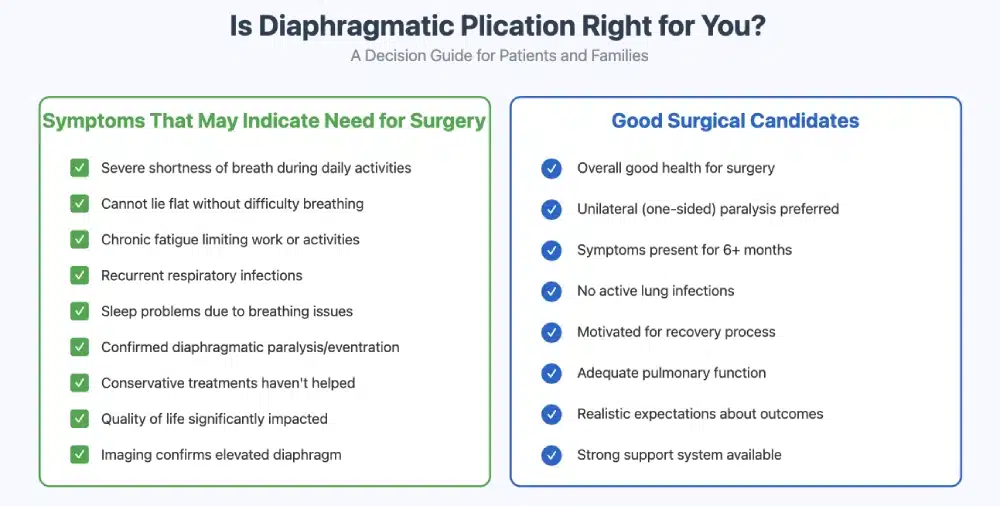
Who Needs Diaphragmatic Plication?
You might be a candidate for diaphragmatic plication if you’re experiencing:
- Severe shortness of breath, especially when lying flat or during physical activity
- Chronic fatigue that limits your daily activities
- Recurrent pneumonia or respiratory infections
- Sleep disturbances due to breathing difficulties
- Reduced exercise tolerance affects your quality of life
Your medical team will consider several factors when determining if plication is right for you:
- The severity of your symptoms
- How long you had the condition
- Your overall health and fitness for surgery
- Whether conservative treatments have been unsuccessful
- The results of pulmonary function tests and imaging studies
The Plication Procedure: What to Expect
Understanding what happens during your surgery can help reduce anxiety and prepare you for the journey ahead.
Pre-Surgical Preparation
Your surgical team will work closely with you in the weeks leading up to your procedure. This typically includes:
- Comprehensive medical evaluation, including heart and lung function tests
- Pulmonary rehabilitation to optimise your breathing capacity
- Nutritional assessment to ensure you’re in the best possible condition for healing
- Smoking cessation support, if needed, as smoking significantly impacts healing
Surgical Approaches
There are several ways your surgeon can perform diaphragmatic plication:
- Thoracotomy (Open Surgery): The traditional approach involves making an incision in your chest wall to directly access the diaphragm. While this requires a larger incision, it provides excellent visualisation and control for complex cases.
- Video-Assisted Thoracoscopic Surgery (VATS): This minimally invasive approach uses small incisions and a camera to guide the surgery. VATS often results in less pain, shorter hospital stays, and faster recovery.
- Robotic-Assisted Surgery: Robotic-assisted surgery may be used in certain cases, offering enhanced precision when performed by experienced surgeons.
During the Surgery
The procedure typically takes 2-4 hours, depending on the complexity of your case. Your surgeon will:
- Position you under general anaesthesia
- Access your chest cavity through the chosen surgical approach
- Identify the weakened or paralysed portion of your diaphragm
- Create carefully placed folds (plications) in the diaphragm muscle
- Secure these folds with strong, permanent sutures
- Ensure proper positioning and tension
- Place temporary drainage tubes to remove air and fluid
- Close the incisions
Recovery: Your Path Back to Better Breathing
Recovery from diaphragmatic plication is a journey that requires patience, but most patients begin to notice improvements in their breathing within days to weeks after surgery.
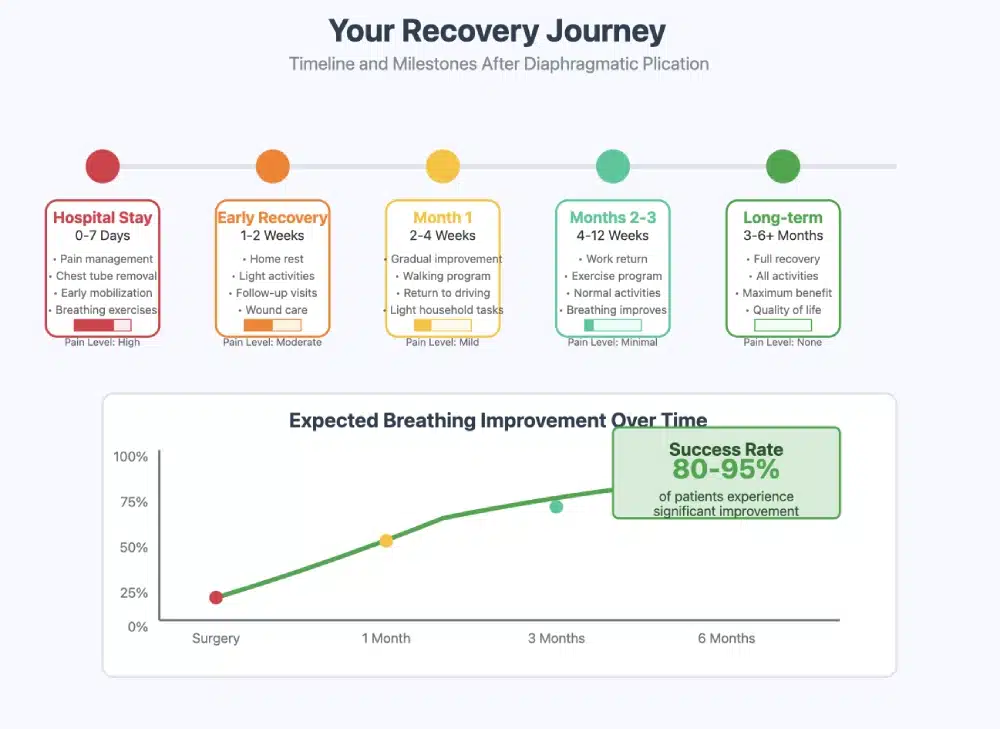
Immediate Post-Operative Period (Hospital Stay)
Your hospital stay will typically last 3-7 days, depending on your surgical approach and individual healing. During this time:
- Pain management is a priority, with medications and techniques tailored to your needs
- Breathing exercises and early mobilisation help prevent complications
- Chest tubes will drain fluid and air, usually removed within 2-3 days
- Gradual activity increase as tolerated, starting with sitting and walking
The First Month at Home
This is a critical period for healing and establishing new patterns:
- Follow your activity restrictions – typically no lifting over 10 pounds
- Practice breathing exercises as taught by your respiratory therapist
- Take medications as prescribed, including pain management and infection prevention
- Attend all follow-up appointments for wound care and progress monitoring
Long-Term Recovery (2-6 Months)
Most patients see continued improvement during this period:
- Gradual return to normal activities, including work and exercise
- Ongoing pulmonary rehabilitation to maximise breathing capacity
- Regular imaging studies to monitor the position and function of your diaphragm
- Lifestyle modifications to support long-term respiratory health
Success Rates and Outcomes
Studies show diaphragmatic plication has high success rates, with studies showing:
- 80-95% of patients experience significant improvement in breathing
- Dramatic reduction in shortness of breath during daily activities
- Improved exercise tolerance and quality of life
- Reduced risk of respiratory infections
- Better sleep quality and energy levels
Long-Term Prognosis
Most patients maintain their breathing improvements for many years after surgery. While the repaired diaphragm may not function exactly like a healthy one, the plication creates a stable platform that significantly improves respiratory mechanics.
Potential Risks and Complications
Like any surgery, diaphragmatic plication carries some risks. It’s important to discuss these openly with your surgeon:
Common, Minor Complications:
- Temporary pain at the incision site
- Mild bleeding or bruising
- Short-term changes in voice (if the recurrent laryngeal nerve is affected)
Less Common, Serious Complications:
- Infection requiring additional treatment
- Bleeding requiring a blood transfusion
- Injury to surrounding organs
- Persistent air leak from the lung
Rare but Serious Complications:
- Heart rhythm problems
- Stroke or blood clots
- Failure of the plication requires additional surgery
Your surgical team will take every precaution to minimise these risks, and most patients experience uncomplicated recoveries.
Alternatives to Surgical Plication
Before considering surgery, your medical team may explore other treatment options:
- Conservative Management:
- Pulmonary rehabilitation and breathing exercises
- Non-invasive ventilation support at night
- Treatment of underlying conditions
- Lifestyle modifications
- Diaphragmatic Pacing: For some patients with phrenic nerve injury, electrical stimulation of the nerve may be an option.
- Supportive Care: In some cases, managing symptoms without surgery may be the best approach, particularly for patients with significant other health conditions.
Choosing the Right Surgeon and Medical Center

The success of your diaphragmatic plication depends significantly on the expertise of your surgical team. When choosing a surgeon, consider:
Experience and Specialisation:
- It’s helpful to choose a thoracic surgeon with regular experience in diaphragmatic procedures.
- Ask about their experience with your specific condition
- Inquire about their success rates and complication rates
Hospital Quality Measures:
- Choose a center with experience in complex thoracic procedures
- Look for hospitals with robust respiratory therapy programs
- Consider centers with dedicated thoracic surgery units
Multidisciplinary Support:
- Ensure access to pulmonologists, respiratory therapists, and rehabilitation specialists.
- Look for centers that offer comprehensive pre- and post-operative care
- Consider the availability of support services for patients and families
Life After Diaphragmatic Plication
Many patients describe life after successful diaphragmatic plication as “getting their life back.” While everyone’s experience is unique, common improvements include:
Physical Improvements:
- Easier breathing during daily activities
- Ability to lie flat comfortably
- Improved exercise tolerance
- Reduced fatigue and increased energy
Emotional and Social Benefits:
- Decreased anxiety about breathing
- Renewed confidence in physical abilities
- Improved relationships and social engagement
- Better overall quality of life
Return to Activities
Most patients can gradually return to their previous activities, including:
- Work and professional responsibilities
- Exercise and recreational activities
- Travel and social engagements
- Hobbies and interests
Supporting Your Recovery: Tips for Patients and Families
For Patients:
- Be patient with your recovery – healing takes time
- Follow your medical team’s instructions carefully
- Stay active within your limitations
- Communicate openly about your symptoms and concerns
- Join support groups for patients with similar conditions
For Family Members:
- Provide emotional support without being overprotective
- Help with practical matters during early recovery
- Encourage adherence to medical recommendations
- Learn about the condition and treatment to better understand the journey
- Take care of your own emotional needs during this stressful time
Financial Considerations and Insurance Coverage
Understanding the financial aspects of your treatment is important for planning:
- Insurance Coverage: Most insurance plans, including Medicare, cover diaphragmatic plication when it’s medically necessary. Work with your healthcare team and insurance company to understand your coverage.
- Cost Factors: The total cost includes surgeon fees, hospital charges, anaesthesia, and follow-up care. Minimally invasive approaches can sometimes lower costs because of shorter hospital stays.
- Financial Assistance: Many hospitals offer financial counseling and assistance programs for patients who need help managing medical expenses.
Research and Future Developments
The field of diaphragmatic surgery continues to evolve, with exciting developments on the horizon:
- Minimally Invasive Techniques: Continued refinement of robotic and thoracoscopic approaches.
- Tissue Engineering: Research into biological materials to enhance diaphragmatic repair.
- Nerve Regeneration: Studies on promoting phrenic nerve healing and regeneration.
- Enhanced Recovery Protocols: Development of optimised care pathways to improve outcomes
Conclusion: Breathing Easy Again

Diaphragmatic plication offers real hope for patients struggling with the debilitating effects of diaphragmatic paralysis or eventration. While the decision to have surgery is never easy, for many patients, it represents the path back to a fuller, more active life.
Remember that you are not alone in this journey. Your medical team, family, and fellow patients who have walked this path are all resources for support and encouragement. With proper preparation, skilled surgical care, and committed recovery efforts, most patients find that diaphragmatic plication gives them something invaluable: the ability to breathe easily again.
The road to recovery requires patience and dedication, but the destination – improved breathing, increased energy, and renewed quality of life – makes the journey worthwhile. Trust in your medical team, believe in your body’s ability to heal, and look forward to the brighter, more breathable future that lies ahead.
This information is provided for educational purposes and should not replace consultation with qualified medical professionals. Always discuss your specific situation with your healthcare team to determine the best treatment approach for your individual needs.
FAQs
What are the Cost and Insurance Options?
1. Surgery Type (Minimally Invasive vs. Open Surgery)
- The cost for keyhole surgery typically ranges from £15,000 to 40,000, including surgeon fees, anesthesia, and hospital charges. Robotic-assisted surgery can be more expensive due to the advanced technology involved, with costs ranging from £25,000 to 50,000.
- Open surgery, which may require a longer hospital stay and intensive care unit stay, can cost between £30,000 to 60,000 or more, depending on the complexity of the surgery.
2. Surgeon’s Fees
The surgeon’s fees will vary based on their level of expertise and geographic location. Surgeons in urban areas or those with specialized expertise in thoracic surgery or diaphragmatic disorders may charge more for their services. These fees can range from £5,000 to £15,000, depending on the complexity of the case and the surgeon’s experience.
3. Anesthesia Fees
Anesthesia fees are another factor in the total cost of the procedure. For general anesthesia, the cost can range from £1,000 to 3,000, depending on the duration of the surgery and the anesthesiologist’s fee.
4. Preoperative and Postoperative Care
- Preoperative evaluations (including imaging tests like X-rays, CT scans, or MRI scans) may add £500 to 3,000to the total cost of the surgery.
- Postoperative care, including follow-up visits, medication, and possible physical therapy, may cost an additional £1,000 to £5,000.
Is Surgery Right for You?
It is an effective treatment for patients with diaphragmatic dysfunction, including conditions like diaphragmatic eventration, paralysis, and weakness. The procedure is particularly beneficial for patients who experience severe respiratory distress and have not found relief from conservative treatments like ventilatory support or respiratory therapy.
If you are struggling with breathing difficulties due to diaphragmatic dysfunction, consult with a thoracic surgeon or pulmonary specialist to determine whether this type of surgery is the right solution for you. Your healthcare provider will evaluate your overall health, the extent of diaphragmatic dysfunction, and other factors to ensure that the surgery provides the best possible results.