If you or a loved one has been diagnosed with a chest wall deformity, you’re not alone. Millions of people worldwide live with conditions like pectus excavatum (sunken chest) or pectus carinatum (protruding chest), and modern medicine offers more treatment options than ever before. This comprehensive guide will walk you through everything you need to know about chest wall deformities, from understanding your diagnosis to exploring both surgical and non-surgical treatment options that can help you feel confident and comfortable in your own body.
What Are Chest Wall Deformities or Pectus Deformities?
Chest wall deformities are structural abnormalities of the chest that can affect both appearance and function. These conditions occur when the costal cartilage connecting the ribs to the breastbone (sternum) grows abnormally, causing the chest to have an unusual shape. While many people think of these as purely cosmetic concerns, chest wall deformities can sometimes affect breathing, heart function, and overall quality of life.
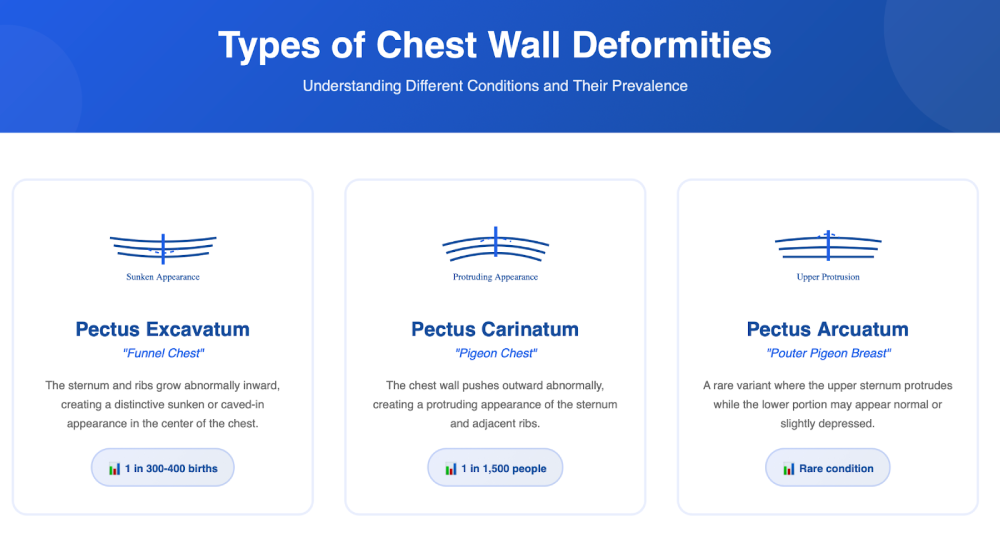
The most common types of chest wall deformities include pectus excavatum, which creates a sunken or caved-in appearance of the chest, and pectus carinatum, where the chest protrudes outward. Less common conditions include pectus arcuatum, Poland syndrome, Jeune syndrome, and traumatic deformities like flail ribs. Each condition is unique, and understanding your specific diagnosis is the first step towards finding the right treatment approach.
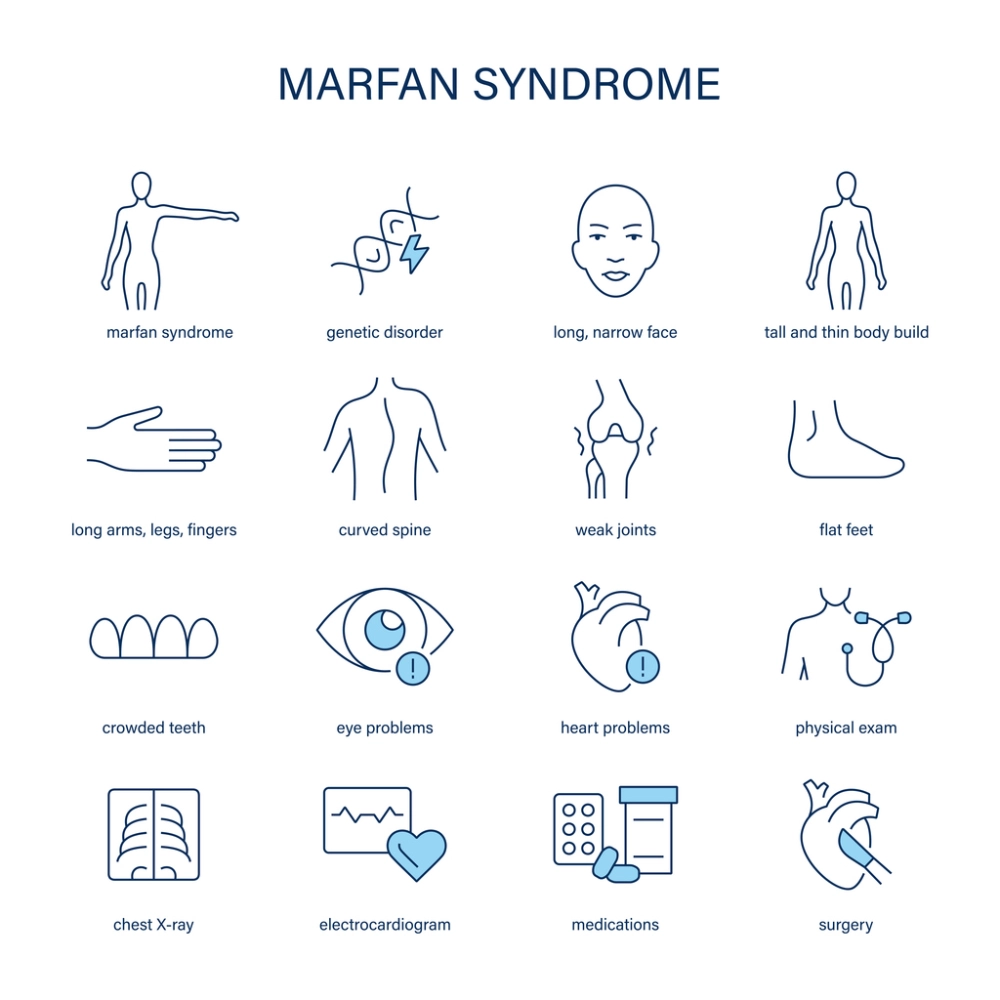
What makes chest wall deformities particularly challenging is their visibility. Unlike many medical conditions that remain hidden, chest wall deformities can affect how you feel about your appearance, potentially impacting self-esteem, social interactions, and participation in activities like swimming or sports. The good news is that whether you’re seeking treatment for medical reasons or to improve your quality of life, there are effective options available. Chest wall deformities are often associated with scoliosis and connective tissue disorders like Marfan syndrome. They become particularly evident and can progress significantly during puberty.
Pectus Excavatum: When Your Chest Caves Inward
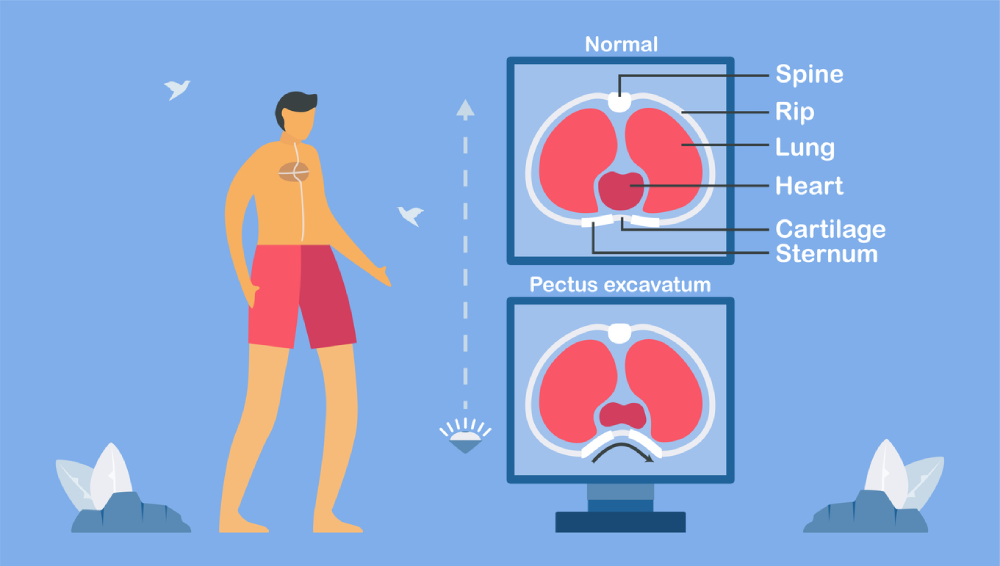
Pectus excavatum, sometimes also called “funnel chest” or “sunken chest,” is the most common chest wall deformity, affecting approximately 1 in 300-400 births. This condition occurs when the sternum and several ribs grow abnormally, creating a depression in the center of the chest. The severity can range from a mild indentation that’s barely noticeable to a deep depression that can affect heart and lung function.
Living with pectus excavatum can be challenging, especially during adolescence when body image concerns are heightened. Many patients report feeling self-conscious about their appearance, avoiding activities that require removing their shirt, or experiencing shortness of breath during exercise. These feelings are completely valid, and it’s important to know that help is available.
The impact of pectus excavatum extends beyond appearance. In moderate to severe cases, the inward curve of the chest can compress the heart and lungs, leading to reduced exercise tolerance and decreased lung capacity. Patients might experience symptoms like rapid heartbeat, shortness of breath during exercise, chest pain, or fatigue. Some people also report feeling their heart “flutter” or experiencing irregular heartbeats, especially when lying on their left side.
Non-Surgical Treatment Options for Pectus Excavatum

For mild cases of pectus excavatum, non-surgical treatments can be effective, especially when started early. The vacuum bell therapy has gained popularity as a non-invasive treatment option. This device creates suction over the depressed area, gradually pulling the sternum forward over time. Patients typically use the vacuum bell for 30 minutes to several hours daily, and improvements can be seen within months of consistent use.
Physical therapy and targeted exercises form another cornerstone of non-surgical treatment. While exercises alone cannot correct the structural deformity, they can significantly improve posture, strengthen the chest muscles, and enhance overall appearance. A specialised physical therapist can design a program focusing on exercises that expand the chest cavity, improve breathing mechanics, and build confidence through better body positioning.
Breathing exercises and respiratory therapy can help maximise lung function and reduce symptoms. Deep breathing techniques, yoga, and swimming are particularly beneficial as they encourage full lung expansion and strengthen the muscles involved in respiration. Many patients find that regular practice of these techniques not only improves their physical symptoms but also helps manage anxiety related to their condition.
Custom-fitted compression garments and chest braces represent another non-surgical approach, particularly effective for younger patients whose bones are still growing. These devices apply gentle, consistent pressure to help guide chest development. While results vary, many families find this option appealing as it avoids the risks associated with surgery.
Surgical Correction: The Nuss and Ravitch Procedures
When non-surgical treatments aren’t sufficient or the deformity is severe, surgical correction offers definitive treatment. The Nuss procedure, a minimally invasive repair of pectus excavatum (MIRPE), has revolutionised treatment since its introduction. This procedure involves inserting one or more curved metal bars beneath the sternum through small incisions on the sides of the chest. The bars push the sternum forward into a normal position and remain in place for 2-3 years while the chest wall remodels.
The Nuss procedure typically takes 1-2 hours, and most patients stay in the hospital for 3-5 days. Recovery involves managing pain, which can be significant initially but improves over the weeks. Most patients return to light activities within 4-6 weeks and full activities, including sports, within 3 months. The success rate is excellent, with over 95% of patients achieving good to excellent cosmetic results.
The Ravitch procedure, an older but still valuable technique, involves removing the abnormal cartilage and repositioning the sternum. This open surgery requires a larger incision across the chest but may be preferred for certain patients, particularly adults with rigid chest walls or those with asymmetric deformities. Some surgeons use a modified Ravitch technique that incorporates a support bar similar to the Nuss procedure.
The choice between surgical techniques depends on various factors, including age, severity of the deformity, chest wall flexibility, and the surgeon’s expertise. During your consultation, your surgeon will discuss which approach best suits your specific situation. Many patients find it helpful to connect with others who have undergone these procedures through support groups or online communities to hear firsthand experiences.
Pectus Carinatum: Managing a Protruding Chest
Pectus carinatum, commonly known as “pigeon chest,” occurs when the chest wall pushes outward, creating a protruding abnormality. This condition affects about 1 in 1,500 people and is more common in males. Unlike pectus excavatum, pectus carinatum rarely causes functional problems with the heart or lungs, but the cosmetic impact can be significant, particularly during the teenage years when peer acceptance feels crucial.
The protrusion in pectus carinatum can be symmetric, affecting the center of the chest equally, or asymmetric, where one side protrudes more than the other. Some patients have a mixed deformity with both excavatum and carinatum components. The condition often becomes more noticeable during growth spurts in adolescence, which is also when many patients first seek treatment.
Understanding that pectus carinatum is not your fault is important. This condition results from abnormal growth of the costal cartilages, not from anything you did or didn’t do. Many successful people, including athletes and celebrities, have lived with pectus carinatum, though modern treatment options mean you don’t have to simply accept the condition if it bothers you.
Bracing: The First-Line Treatment for Pectus Carinatum

Chest wall bracing has emerged as a highly effective non-surgical treatment for pectus carinatum, particularly in children and adolescents whose chest walls are still flexible. Custom-made compression braces apply controlled pressure to the protruding area, gradually reshaping the chest wall over time. Studies show excellent results when patients follow the treatment plan closely.
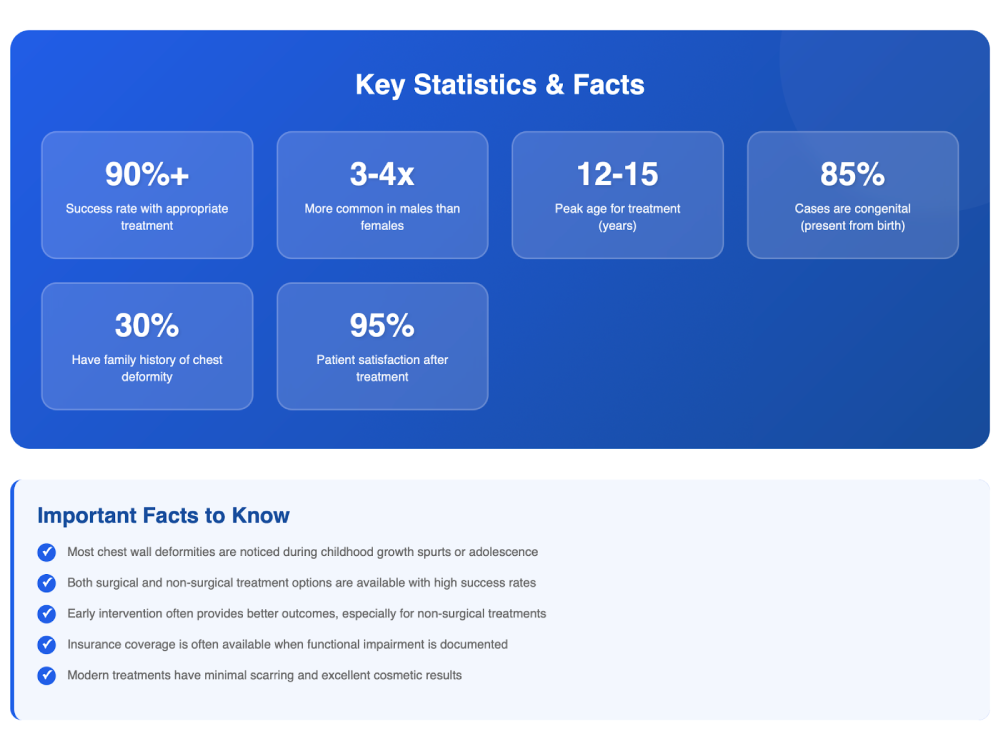
The bracing protocol typically involves wearing the device for 14-23 hours daily, though some newer dynamic compression systems require less wearing time. Initial measurements and fittings ensure the brace applies appropriate pressure without causing discomfort or skin problems. Regular follow-up appointments allow for adjustments as the chest shape improves. Most patients see noticeable improvement within 3-6 months, with full correction often achieved within 12-24 months.
Modern braces are designed to be worn discreetly under clothing, allowing patients to maintain normal activities, including school and most sports. Some patients initially feel self-conscious about wearing a brace, but most quickly adapt and appreciate avoiding surgery. The key to success is compliance – wearing the brace as prescribed even when improvements make it tempting to stop early.
For patients who find traditional bracing uncomfortable or impractical, newer treatment options include adjustable dynamic compression systems that can be worn for shorter periods with similar effectiveness. These systems use precise pressure measurements to optimise treatment while minimising wearing time, making compliance easier for busy teenagers and young adults.
Surgical Options for Pectus Carinatum
While bracing successfully treats most pectus carinatum cases, surgery remains an option for patients with severe deformities, those who don’t respond to bracing, or adults whose chest walls are too rigid for conservative treatment. The modified Ravitch procedure is the most common surgical approach, involving the removal of the abnormal cartilage and repositioning of the sternum.
The surgical procedure typically takes 2-4 hours and requires a hospital stay of 3-5 days. Surgeons make an incision across the chest, remove the deformed cartilage segments, and may place a small bar behind the sternum for support during healing. Recovery involves managing post-operative pain and gradually returning to normal activities over 6-12 weeks. Most patients achieve excellent cosmetic results with high satisfaction rates.
Minimally invasive techniques for pectus carinatum are being developed, including the Abramson procedure, which uses a compression bar placed externally to gradually reshape the chest. These newer approaches aim to reduce surgical trauma and recovery time while maintaining excellent results. Your surgeon can discuss whether you’re a candidate for these innovative techniques.
The decision to pursue surgery should be made carefully with your medical team, considering factors like the severity of your deformity, your age, the impact on your quality of life, and your personal goals. Many patients benefit from psychological counseling before and after surgery to address body image concerns and set realistic expectations for outcomes.
Pectus Arcuatum and Mixed Deformities
Pectus arcuatum, also called currarino-silverman syndrome or pouter pigeon breast, is a rare chest wall deformity characterised by protrusion of the upper sternum and adjacent cartilages. This creates a distinctive appearance where the upper chest bows outward while the lower portion may appear normal or even slightly depressed. Though less common than pectus excavatum or carinatum, this condition can be equally distressing for affected individuals.
Mixed or complex chest wall deformities combine features of different conditions, such as excavatum on one side and carinatum on the other, or varying degrees of asymmetry. These complex cases require careful evaluation and often benefit from customised treatment approaches. Advanced imaging techniques like 3D CT scanning help surgeons plan precise corrections for these challenging deformities.
Treatment for pectus arcuatum and mixed deformities often requires a combination approach. Younger patients might start with bracing or vacuum therapy to address the prominent areas while using exercises to strengthen surrounding muscles. When surgery is necessary, procedures are tailored to address each component of the deformity, sometimes requiring innovative techniques or combinations of established procedures.
The psychological impact of rare or complex chest wall deformities can be significant, as patients may feel isolated or struggle to find others with similar experiences. Connecting with specialised treatment centers and online support communities can provide valuable resources and emotional support. Remember that even complex deformities can be successfully treated with the right approach and an experienced medical team.
Choosing the Right Treatment Center
Selecting the right treatment center and medical team is crucial for achieving the best outcomes in chest wall deformity treatment. It’s helpful to choose a center with experience in chest wall deformities, where surgeons regularly perform these procedures and care teams can provide full evaluation and treatment options.
A quality treatment center should offer multidisciplinary care, including thoracic surgeons, paediatric specialists for younger patients, anaesthesiologists experienced in chest wall surgery, physical therapists, and psychological support services. The team should take time to understand your specific concerns, explain all treatment options thoroughly, and help you make an informed decision that aligns with your goals and lifestyle.
Consider practical factors when choosing a treatment center, including insurance coverage, travel requirements for follow-up care, and the center’s support services. Many insurance plans cover chest wall deformity treatment when there’s documented functional impairment, though coverage for purely cosmetic concerns varies. The treatment center’s financial counselors should help navigate insurance approval and discuss payment options if needed.
Don’t hesitate to seek second opinions, especially for complex cases or if you’re unsure about the recommended treatment approach. Reputable surgeons welcome second opinions and understand that chest wall deformity treatment is a significant decision. Virtual consultations have made it easier to connect with specialists regardless of geographic location, expanding access to expert care.
The Cost of Treatment: Insurance and Financial Considerations
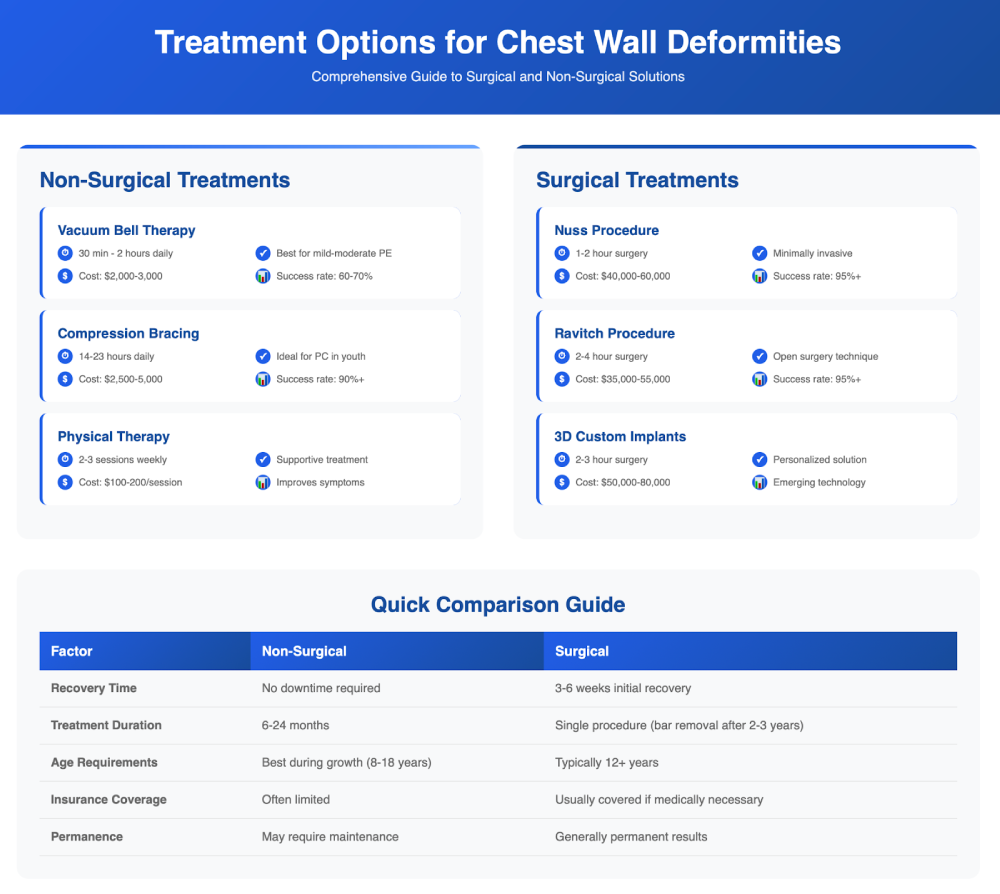
Understanding the financial aspects of chest wall deformity treatment helps you plan effectively and avoid unexpected costs. Treatment costs vary widely depending on the approach chosen, ranging from hundreds of dollars for bracing to tens of thousands for surgical procedures. Costs vary widely depending on the approach—from a few thousand pounds for bracing to significantly more for surgery.
Insurance coverage for chest wall deformity treatment has improved significantly as medical understanding of these conditions’ functional impacts has grown. Most insurance plans cover treatment when there’s documented cardiopulmonary impairment, with specific criteria varying by insurer. Common covered indications include a Haller index greater than 3.25 for pectus excavatum, documented cardiac compression, reduced pulmonary function, or exercise intolerance.
The insurance approval process typically requires comprehensive documentation, including physical examination findings, imaging studies (CT or MRI), pulmonary function tests, and sometimes cardiac evaluation. Your medical team should be experienced in working with insurance companies and can help compile the necessary documentation. Some centers have dedicated insurance specialists who handle prior authorisations and appeals if initial requests are denied.
For patients without insurance or whose plans don’t cover treatment, various financial options exist. Many hospitals offer payment plans, financial assistance programs, or cash discounts. Some patients explore medical tourism for more affordable surgical options, though this requires careful research to ensure quality and safety. Crowdfunding has also helped some families raise funds for treatment. Remember that investing in treatment that improves your quality of life and confidence can be invaluable.
Living with Chest Wall Deformities: Emotional and Psychological Support

The emotional impact of living with a chest wall deformity often equals or exceeds the physical challenges. Many patients experience anxiety, depression, social withdrawal, or body dysmorphic concerns related to their condition. These feelings are entirely normal and valid – your emotional well-being is just as important as your physical health.
Adolescents and young adults may face particular challenges as they navigate dating, sports participation, and social situations that involve removing their shirt. The fear of judgment or questions about their appearance can lead to avoidance behaviours that limit life experiences. Professional counseling can provide valuable coping strategies and help build confidence regardless of whether you choose treatment.
Support groups, both in-person and online, connect you with others who understand your experience firsthand. These communities offer practical advice, emotional support, and inspiration from those who’ve successfully navigated treatment. Many patients find that sharing their story and helping others reduces their own anxiety and builds resilience.
Family support plays a crucial role in treatment success, particularly for younger patients. Parents should maintain open communication, validate their child’s concerns without minimising them, and involve them in treatment decisions appropriately. Siblings may also need support to understand the condition and treatment process. Family therapy can help navigate the challenges that chest wall deformities present to the entire family system.
Recovery and Rehabilitation: Your Journey to Healing
Recovery from chest wall deformity treatment, whether surgical or non-surgical, requires patience, dedication, and proper support. The recovery timeline varies depending on the treatment type, your age, and overall health. Understanding what to expect helps you prepare mentally and practically for the journey ahead.
For surgical patients, the immediate post-operative period focuses on pain management and preventing complications. Modern pain control techniques, including nerve blocks, epidural catheters, and multimodal analgesia, have significantly improved the recovery experience.
Most patients are walking within 24 hours of surgery and are discharged home within 3-5 days.
The first two weeks at home require significant rest and assistance with daily activities.
Physical therapy begins early in the recovery process, initially focusing on breathing exercises and a gentle range of motion activities. As healing progresses, therapy advances to posture training, core strengthening, and gradual return to normal activities. Most patients return to school or work within 3-4 weeks and resume sports after 3 months, though contact sports may be restricted longer.
Non-surgical treatments like bracing or vacuum bell therapy require their own form of dedication. Success depends on consistent use and regular follow-up appointments for adjustments. Many patients find it helpful to establish routines that incorporate treatment into daily life, such as wearing the vacuum bell while studying or watching TV. Keeping a treatment diary can help track progress and maintain motivation during the months of treatment required.
Advanced Treatment Technologies and Future Directions
The field of chest wall deformity treatment continues to evolve with technological advances improving outcomes and patient experience. 3D printing technology now allows the creation of custom implants and surgical guides that precisely match each patient’s anatomy. These patient-specific implants can achieve better cosmetic results with potentially shorter surgery times and reduced complications.
Magnetic technology represents an exciting frontier in chest wall treatment. The magnetic mini-mover procedure (3MP) uses magnetically controlled implants to gradually remodel the chest wall without the need for invasive surgery. Early results show promise for treating both pectus excavatum and carinatum with minimal scarring and reduced recovery time.
Bioabsorbable materials are being developed for chest wall reconstruction, eliminating the need for bar removal surgeries. These materials provide temporary support while the chest wall heals and remodels, then gradually dissolve as they’re no longer needed. This technology could particularly benefit paediatric patients who would otherwise require multiple surgeries as they grow.
Research into the genetic basis of chest wall deformities may eventually lead to prevention strategies or earlier interventions. Scientists have identified several genetic markers associated with increased risk, though the inheritance pattern remains complex. Understanding these genetic factors could help identify at-risk individuals early and guide treatment timing for optimal results.
Exercise and Physical Activity: Building Strength and Confidence
Physical activity plays a vital role in managing chest wall deformities, both as part of treatment and for overall well-being. While your condition might make you hesitant about exercise, especially activities requiring the removal of your shirt, staying active offers numerous benefits, including improved posture, increased lung capacity, and enhanced self-confidence.
Swimming is particularly beneficial for individuals with chest wall deformities. The water’s buoyancy reduces stress on the chest while providing resistance that strengthens muscles. The breathing patterns required for swimming also help expand lung capacity. Many patients find that regular swimming improves both their physical symptoms and their comfort with their appearance in swimwear.
Strength training, when properly guided, can significantly improve the appearance of chest wall deformities. Exercises targeting the pectoralis major and minor muscles, serratus anterior, and back muscles can create better chest symmetry and improve posture. Working with a physical therapist or certified trainer experienced with chest wall conditions ensures safe and effective exercise progression.
Cardiovascular exercise improves heart and lung function, particularly important for those with pectus excavatum who may have reduced cardiopulmonary capacity. Activities like cycling, rowing, or elliptical training provide excellent cardiovascular benefits while minimising chest wall stress. Gradually increasing exercise intensity helps build endurance and confidence in your body’s capabilities.
Nutrition and Lifestyle Factors
While nutrition alone cannot correct chest wall deformities, proper dietary habits support overall health and can optimise treatment outcomes. Adequate protein intake is essential for tissue healing, particularly important during recovery from surgery or while undergoing growth during bracing treatment. Lean meats, fish, legumes, and dairy products provide the building blocks necessary for tissue repair and muscle development.
Maintaining a healthy body weight reduces stress on the chest wall and can improve the appearance of mild deformities. Being underweight may make chest wall deformities more prominent, while excess weight can complicate surgical procedures and recovery. Work with a nutritionist if you need guidance on achieving and maintaining an optimal weight for your condition.
Posture awareness throughout daily activities significantly impacts how chest wall deformities appear and feel. Poor posture, often developed as an unconscious attempt to hide the deformity, can actually make it more noticeable and contribute to back pain. Ergonomic workstation setup, regular posture checks, and core strengthening exercises help maintain proper alignment.
Avoiding smoking and excessive alcohol consumption is crucial, particularly if considering surgery. Smoking impairs wound healing, increases infection risk, and can compromise lung function – already a concern for many with chest wall deformities. If you smoke, quitting several weeks before surgery significantly improves outcomes. Your medical team can provide resources for smoking cessation support.
When to Seek Treatment: Making the Decision
Deciding when to seek treatment for a chest wall deformity is highly personal and depends on various factors, including severity, symptoms, age, and quality of life impact. There’s no universal “right time” – what matters is finding the approach that aligns with your needs and goals.
For children and adolescents, timing considerations include skeletal maturity, psychological readiness, and the potential for non-surgical interventions. Early intervention with bracing for pectus carinatum often yields better results than waiting until skeletal maturity. However, surgical correction of pectus excavatum is often delayed until the adolescent growth spurt is nearly complete to reduce the risk of recurrence.
Adults seeking treatment should consider their lifestyle, career demands, and support system when planning intervention. While chest walls become less flexible with age, making some treatments more challenging, many adults successfully undergo correction with excellent results. The decision often comes down to whether the physical or psychological impact of the deformity outweighs the temporary disruption caused by the treatment.
Warning signs that warrant prompt medical evaluation include increasing shortness of breath, chest pain, heart palpitations, or progressive worsening of the deformity. These symptoms may indicate that the condition is affecting cardiopulmonary function and requires medical attention. Don’t wait for symptoms to become severe before seeking evaluation – early intervention often provides more treatment options.
Success Stories and Patient Experiences

Real patient experiences provide valuable insight and inspiration for those considering treatment. Mark, a 16-year-old with severe pectus excavatum, underwent the Nuss procedure after years of avoiding sports due to breathing difficulties. Six months post-surgery, he joined his school’s track team and reports feeling “like a completely different person” with improved stamina and confidence.
Sarah, diagnosed with pectus carinatum at age 12, completed 18 months of bracing treatment. Initially self-conscious about wearing the brace, she found that most classmates were supportive once she explained her condition. Now in college, she maintains the correction achieved through bracing and advocates for early intervention through social media.
Adult patients also find success with treatment. Jennifer, a 35-year-old teacher, lived with mild pectus excavatum her entire life before seeking treatment. Though her condition didn’t significantly impact her physical health, the psychological burden had limited her social activities and relationships. After undergoing surgical correction, she reports improved self-esteem and a more active lifestyle.
These stories highlight that success isn’t just measured in physical correction but in improved quality of life, increased confidence, and the ability to pursue activities previously avoided. Each journey is unique, but the common thread is that treatment – whether surgical or non-surgical – can be life-changing when approached with realistic expectations and proper support.
Preparing for Your Consultation
Your first consultation with a chest wall deformity specialist is an important step towards treatment. Preparing thoroughly helps you make the most of this appointment and ensures all your concerns are addressed. Start by documenting your medical history, including any previous treatments attempted, current medications, and family history of chest wall deformities.
Create a list of symptoms you experience, even those that might seem unrelated. Include physical symptoms like shortness of breath or chest pain, as well as psychological impacts such as anxiety or social avoidance. Photos showing the progression of your deformity over time can be helpful for the medical team to assess changes and plan treatment.
Prepare questions for your medical team about treatment options, expected outcomes, risks, recovery time, and costs. Don’t hesitate to ask about the surgeon’s experience with your specific condition, success rates, and whether you can connect with previous patients. Understanding the full scope of treatment helps you make an informed decision.
Bring a trusted friend or family member to your consultation if possible. They can help remember information, ask additional questions, and provide emotional support. Many centers also offer virtual consultations for initial evaluations, making it easier to seek expert opinions regardless of location.
Long-term Outcomes and Follow-up Care
Understanding long-term outcomes helps set realistic expectations for chest wall deformity treatment. Most patients who undergo successful treatment maintain excellent results indefinitely, though some factors can influence long-term outcomes. Regular follow-up care ensures any issues are identified and addressed promptly.
Surgical correction typically provides permanent results, with recurrence rates below 5% for properly performed procedures. The Nuss bar removal after 2-3 years is a minor procedure compared to the initial surgery, and most patients maintain their correction afterward. Long-term studies show high patient satisfaction rates, with over 90% reporting they would undergo the procedure again.
Non-surgical treatments like bracing may require maintenance phases to preserve correction, particularly in younger patients still growing. Some patients need to wear retainer braces at night for several months after achieving correction. This maintenance phase is crucial for preventing recurrence and ensuring lasting results.
Regular follow-up appointments monitor for potential complications and ensure optimal outcomes. These visits typically include physical examination, imaging studies if needed, and assessment of any symptoms. Many patients find that annual check-ups provide peace of mind and help maintain their treatment results. Your medical team will establish a follow-up schedule tailored to your specific treatment and needs.
Conclusion: Your Path Forward
Living with a chest wall deformity presents unique challenges, but you don’t have to face them alone. Whether you’re just beginning to explore treatment options or ready to take the next step, remember that effective treatments exist and thousands of people have successfully improved their condition. The key is finding the right approach for your specific situation and goals.
Take time to thoroughly research your options, connect with experienced medical teams, and consider all aspects of treatment, including physical, emotional, and financial factors. Don’t let fear or embarrassment prevent you from seeking help – medical professionals who specialise in chest wall deformities understand the impact these conditions have and are committed to helping you achieve the best possible outcome.
Remember that treatment success isn’t just about physical correction but about improving your overall quality of life. Whether that means being able to exercise without shortness of breath, feeling confident at the beach, or simply living without the constant awareness of your chest appearance, treatment can help you achieve your goals.
Your journey with a chest wall deformity is unique, but you’re not alone. Support groups, online communities, and medical professionals are available to guide and support you. With today’s modern treatment options, patients have more choices than ever before to address chest wall deformities. Take the first step towards treatment by scheduling a consultation with a specialist who can evaluate your condition and discuss your options. Your future self will thank you for taking action today.
FAQs
What are the different types of chest wall deformities types?
There are different types of congenital chest wall deformities. The most commons is the pectus excavatum, also called in simpler terms funnel chest. In this condition the anterior portion of the chest sinks in and forms like a funnel. There are different variant of it according to the severity of the deformity (mild- moderate and severe) and the shape of it. Some can involve just the bottom part of the chest others the entire breast bone, sometime the defect is wide and long and takes the name of grand-canyon variant. This deformity affects nearly 2/3 of all patients and is more prevalent in males. Another common variant is the pectus carinatum or also called pigeon chest. In this condition the breastbone sticks forward like the bow of a ship. It also has different grades of severity and sometime it can also be visible under clothes. This condition affects about the remaining 1/3 of the cases. Lastly there is a rare variant called pectus arcuatum which is a combination of the two previously mentioned defects. Very often this is wrongly diagnosed as pectus excavatum as the chest does sink in, but, more importantly, it also sticks out. It is very important to be familiar with this condition and having diagnosed properly as the wrong diagnosis might lead to the wrong treatment.
What are the common chest wall deformity symptoms?
Symptoms varies greatly according to the type and severity of the defect. Some patients with a mild conditions have no physical symptoms at all or are very mildly symptomatic. Others with severe defects can experience shortness of breath and pain along the anterior rib cage, especially after exercise. This pain is quite non-specific and it is mostly related to an asymmetry in the rib cage that responds differently to mechanical stress. Shortness of breath is also rather common, but, unfortunately, it is difficult to diagnose it as most patients are young and fit at rest. The problems only become evident during sub-maximal exercise. In this category of patients a cardiopulmonary exercise test might be the best way forward to document the symptoms. Static lung function is not useful in this scenario, nor is a standard chest x-ray.