Home
Conditions
Understanding pleural biopsy and related procedures is essential for anyone facing lung-related health issues or requiring diagnostic interventions. These terms might sound complex, but they are critical in diagnosing and treating various conditions affecting the pleura, the membrane surrounding the lungs. This guide aims to simplify these procedures and provide a comprehensive overview, helping you know what to expect and how these medical interventions can be beneficial.
A pleural biopsy is a medical procedure where a small sample of tissue from the pleura is removed for examination. This is often done to investigate abnormalities such as infections, tumors, or other pathologies. There are various methods for performing a pleural biopsy, including needle biopsy, thoracoscopy, or video-assisted thoracoscopic surgery (VATS). Each technique has its own advantages and is chosen based on the patient’s condition and the information needed.
The procedure typically starts with local anesthesia, after which a needle is inserted into the pleural space to collect a tissue sample. In some cases, a small incision may be made if a thoracoscopic approach is used. Patients usually undergo imaging studies, such as ultrasound or CT scans, to guide the physician in locating the area of concern accurately.
Pleural biopsies are performed for several reasons. One of the primary motivations is to identify the cause of pleural effusion, where excess fluid accumulates between the pleura layers. This condition can result from various factors, including infection, cancer, or inflammatory diseases.
Other indications for a pleural biopsy include diagnosing specific types of lung cancer, assessing the stage of cancer, and evaluating non-cancerous conditions such as tuberculosis or mesothelioma. Ultimately, the biopsy provides critical information that can influence treatment decisions and improve patient outcomes.
Patients undergoing a pleural biopsy can expect the procedure to last from 30 to 90 minutes, depending on the method used. Generally, the experience is outpatient, meaning patients can go home the same day. Before the procedure, medical professionals will explain the process and address any concerns.
After the biopsy, patients are usually monitored for a short time to check for complications. It’s normal to experience some discomfort or mild pain at the biopsy site, which can often be managed with over-the-counter pain relief medications. Overall, the procedure is minimally invasive, making it a preferred approach for diagnosing pleural conditions.
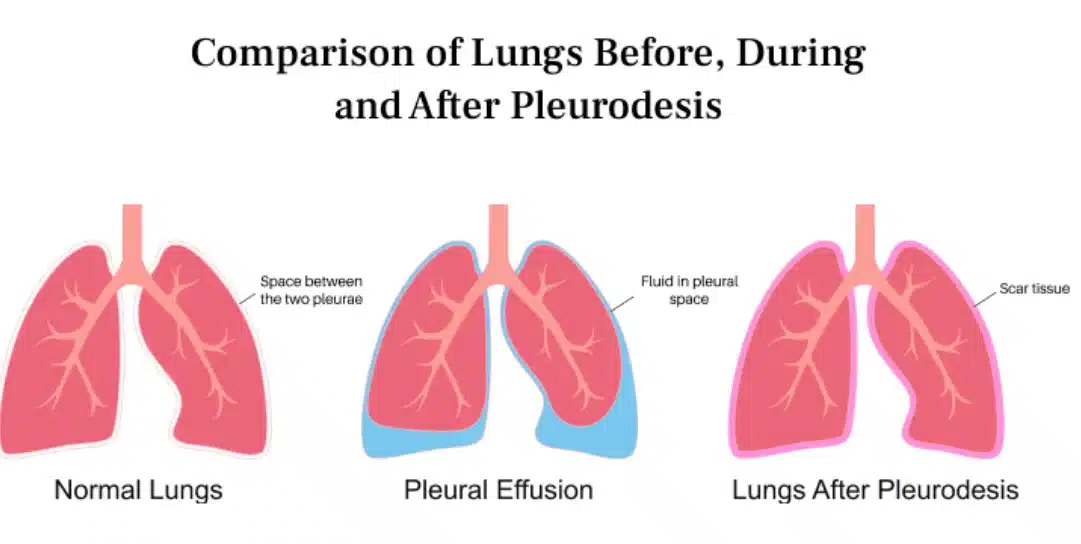
This procedure is used to eliminate the pleural space, preventing the accumulation of fluid or air. It’s especially beneficial for patients suffering from recurrent lung issues or pneumothorax. By creating an inflammatory response, it causes the pleura layers to adhere to each other, effectively stopping fluid collection.
The primary goal of pleurodesis is to relieve symptoms and improve the quality of life for patients with chronic lung conditions. It’s often recommended when other treatments have failed or are inappropriate. Understanding this procedure can help patients make informed decisions about their treatment options.
There are several methods to perform pleurodesis, including chemical pleurodesis and mechanical pleurodesis. Chemical pleurodesis involves instilling a sclerosing agent through a chest tube or during surgery. Common agents used include talc, doxycycline, or bleomycin. Talc is the most widely used due to its effectiveness and low cost.
Mechanical pleurodesis, on the other hand, is a surgical procedure where the pleural surfaces are physically roughened to induce adhesion. This method may be performed during a thoracotomy or thoracoscopy. The choice of method typically depends on the patient’s overall health and the specific circumstances surrounding their lung condition.
Choosing the appropriate type of pleurodesis requires careful consideration of various factors, including the underlying condition, the patient’s overall health, and previous treatment responses. A thorough evaluation by a healthcare provider is essential in determining the best approach tailored to individual needs.
Patients should engage in open discussions with their doctors about the potential risks and benefits associated with each pleurodesis method. Together, they can weigh these aspects and decide on the most effective treatment plan. Collaborative decision-making plays a crucial role in achieving satisfactory outcomes for patients undergoing pleurodesis.
Like any medical procedure, pleural biopsies and pleurodesis come with potential risks. For pleural biopsy, common risks include bleeding, infection, and injury to surrounding organs. While serious complications are rare, they can occur, emphasizing the importance of having the procedure performed by experienced professionals.
Pleurodesis also carries risks, such as the potential for chest pain, fever, or difficulty breathing post-procedure. In some cases, the pleura may not adhere as intended, leading to the recurrence of fluid accumulation. It’s essential for patients to be well-informed about these risks, as understanding them can help alleviate anxiety and promote better outcomes.
The benefits of undergoing pleural biopsy can be significant. A pleural biopsy is invaluable for diagnosing serious conditions, providing clarity that can lead to appropriate treatment plans. By identifying the underlying cause of pleural effusion or lung abnormalities, this procedure paves the way for targeted therapies.
Pleurodesis offers substantial advantages for patients suffering from chronic pleural effusions. By preventing future fluid accumulation, it can significantly enhance quality of life and reduce the frequency of hospital visits. Many patients report relief from symptoms such as breathlessness and discomfort, making it a worthy consideration for those affected.
By opting for pleurodesis, patients may experience improved respiratory function and a decrease in hospital visits due to recurrent symptoms.
Pleurodesis is an important consideration for patients with recurring pleural effusions, as it can effectively prevent fluid buildup in the pleural space.
When considering a pleural biopsy or pleurodesis, patients must weigh the potential risks against the anticipated benefits. It’s crucial to engage in thorough discussions with healthcare providers to gain a nuanced understanding of how these procedures can impact individual health outcomes.
Ultimately, the decision should reflect the patient’s values and preferences alongside medical advice. Knowledge is power, and being well-informed about both the advantages and potential drawbacks of these procedures can lead to more satisfactory health decisions.
Pleural biopsy and pleurodesis are essential medical procedures designed to diagnose and treat conditions affecting the pleura and lungs. By understanding these interventions, patients can better navigate their health journeys and collaborate with healthcare providers to make informed decisions. The complexities of lung health can be daunting, but being proactive and educated can significantly impact treatment outcomes.
With ongoing advancements in medical technology and techniques, the future of pleural procedures promises to be even more effective and patient-centric. As always, maintaining an open dialogue with healthcare professionals and staying informed about one’s health is key to optimal care.
A pleural biopsy is a medical procedure where a small tissue sample is taken from the pleura, the membrane surrounding the lungs, to help diagnose conditions like infections or tumors.
Individuals may require a pleural biopsy to investigate the cause of pleural effusion, diagnose lung cancer, or assess other lung-related conditions.
Pleurodesis is a procedure that eliminates the pleural space to prevent fluid or air accumulation, often used in cases of recurrent pleural effusions.
Yes, both procedures carry risks, including bleeding, infection, and complications related to anesthesia. However, serious complications are relatively rare.
Pleurodesis can provide significant relief from symptoms like breathlessness and reduce the need for frequent medical interventions related to fluid accumulation.
Ready to receive expert lung and chest treatments in London? Contact our specialist thoracic surgeon today to schedule your consultation and take the first step toward better health. Your well-being is our priority—reach out now!
Mr. Marco Scarci is a highly respected consultant thoracic surgeon based in London. He is renowned for his expertise in keyhole surgery, particularly in the treatment of lung cancer and pneumothorax (collapsed lung). He also specialises in rib fractures, hyperhidrosis (excessive sweating), chest wall deformities and emphysema.
Mr. Marco Scarci is a highly respected consultant thoracic surgeon based in London.