Home
Conditions
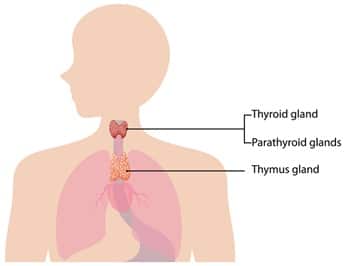
Thymic cancer refers to malignancies that originate in the thymus, a small organ located in the upper chest, behind the sternum. The thymus plays a crucial role in the immune system, particularly in the development and maturation of T-cells, which are essential components of the immune response. Two primary subtypes of thymic cancer are identified: thymoma and thymic carcinoma, each exhibiting distinct characteristics and clinical behaviors.
Thymoma is generally considered the more common of the two, characterized by slow growth and a better prognosis. It arises from the epithelial cells of the thymus and often presents in patients with autoimmune disorders, underscoring its association with immune system dysregulation. Common histological subtypes include type A, type AB, type B1, type B2, and type B3 thymomas, each differing in cellular composition and potential for aggressive behavior.
Thymoma is also frequently studied in research for its unique characteristics among thymic cancers.
Thymoma is crucial to understanding the broader spectrum of thymic cancer.
Understanding the nuances between thymoma and thymic carcinoma is essential for effective treatment strategies.
In contrast, thymic carcinoma is notably rarer and tends to be more aggressive, often associated with a poorer prognosis. This subtype arises from the more malignant transformation of the thymic epithelial cells. Thymic carcinoma is typically classified based on its histological features, including a higher degree of anaplasia and atypical cellular structures, making it more difficult to treat effectively compared to thymoma.
The presence of thymic cancer can significantly impact overall health, leading to complications related to the immune system and potentially affecting the patient’s quality of life. Symptoms may include chest pain, cough, and shortness of breath, reflecting the growing tumor’s pressure on surrounding structures. Understanding the nature and differences between thymoma and thymic carcinoma is essential for appropriate management and treatment of individuals affected by these conditions.
Thymic cancer, categorized primarily into thymoma and thymic carcinoma, has not been fully elucidated in terms of its exact causes. Nevertheless, a complex interplay of genetic predispositions and environmental factors has been identified as influencing its development. Genetic susceptibility can play a pivotal role, with certain inherited conditions significantly increasing the risk. For instance, those with syndromes such as Li-Fraumeni and neurofibromatosis type 1 are at a heightened likelihood of developing thymic malignancies.
This correlation emphasizes the importance of monitoring patients with autoimmune disorders for potential thymoma development.
Awareness of the signs and symptoms of thymoma can lead to earlier diagnosis and treatment.
Environmental factors may also contribute to the onset of thymic cancer. Exposure to certain chemicals, radiation, or a history of viral infections has been proposed as potential contributors to the development of thymoma and thymic carcinoma. However, specific environmental triggers remain largely speculative, requiring further comprehensive research to establish definitive links.
Additionally, there exists a correlation between autoimmune diseases and thymic cancer. Conditions such as Myasthenia Gravis, an autoimmune disorder that impacts neuromuscular function, frequently coexist with thymic tumors. Approximately 10-15% of individuals diagnosed with thymoma also suffer from Myasthenia Gravis, revealing a significant association between these conditions. Other autoimmune disorders, including systemic lupus erythematosus and rheumatoid arthritis, have also been noted in patients with thymic cancer, suggesting shared underlying mechanisms that may predispose individuals to both autoimmune dysfunctions and thymic malignancies.
Risk factors are further complicated by demographic trends, as thymic cancer typically presents more frequently in adults, particularly within the fourth and fifth decades of life. Understanding these multifaceted causes and risk factors is crucial for early detection and improved management of thymic cancer. Continued exploration into the genetic, environmental, and autoimmune connections will provide invaluable insights into preventing and treating thymoma and thymic carcinoma effectively.
Thymic cancer, comprising primarily thymoma and thymic carcinoma, can present a variety of symptoms. These symptoms may differ significantly based on the specific type of tumor, its size, and its location within the thymus gland. Common symptoms associated with thymoma include chest pain, cough, and difficulty breathing, which may arise due to pressure on surrounding structures in the thoracic cavity. Patients may also experience systemic symptoms such as unexplained weight loss, fatigue, and fever. In certain cases, thymoma can lead to paraneoplastic syndromes, where the cancer affects other bodily functions, resulting in symptoms such as myasthenia gravis, which causes muscle weakness. It is essential to recognize that symptoms may not manifest until the tumor has progressed, making early detection challenging.
To accurately diagnose thymic cancer, healthcare professionals employ various diagnostic methods. Initially, imaging tests play a crucial role; computed tomography (CT) scans and magnetic resonance imaging (MRI) are commonly used to visualize the thymus gland and surrounding tissues. These imaging techniques help determine the size and location of the tumor, providing insight into its potential impact on nearby structures. Once a suspicious mass is identified, a biopsy is typically performed to obtain tissue samples. This procedure allows for histopathological examination, which is vital in distinguishing between a thymoma and thymic carcinoma, as well as determining the cancer’s stage.
Furthermore, advanced imaging techniques like positron emission tomography (PET) scans can be utilized to assess the metabolic activity of the tumor and identify any metastases. The combination of imaging studies and biopsy results not only helps confirm a diagnosis but also assists healthcare providers in determining an appropriate treatment plan tailored to the individual patient’s needs. Timely and accurate diagnosis is critical in managing thymic cancer effectively.
Treatment options for thymic cancer, specifically thymoma and thymic carcinoma, vary significantly based on the specific type and stage of cancer, as well as the overall health of the patient. Surgical intervention remains the primary and most effective treatment for localized thymoma. During this procedure, the tumor, and potentially surrounding tissue, is removed, offering the best chance for a complete cure. Surgical resection may not be as effective for thymic carcinoma, which tends to be more aggressive.
In cases where surgical resection is not feasible, or when the cancer has metastasized, additional treatments such as chemotherapy and radiation therapy may be used. Chemotherapy can be administered either alone or in conjunction with surgery, particularly for thymic carcinoma, where systemic treatment is often necessary. This approach utilizes drugs that target rapidly dividing cancer cells, but it also affects healthy cells, leading to various side effects. Conversely, radiation therapy focuses on directing high-energy rays to the tumor site, aiming to kill cancer cells and reduce tumor size, which can be beneficial pre- or post-surgery.
Emerging therapies are also gaining attention in the treatment of thymic cancer. These novel approaches include targeted therapy and immunotherapy, which exploit the body’s immune system to fight cancer or specifically target cancer cells. Clinical trials continue to explore these options to determine their effectiveness compared to conventional treatments.
Prognosis for patients with thymoma generally tends to be positive, particularly when diagnosed earlier and treated promptly. Factors influencing survival rates include tumor stage at diagnosis, histological subtype, and the success of the surgical intervention. Early diagnosis enables more tailored and effective treatment, ultimately improving long-term outcomes for those affected by this rare form of cancer.