Living with thoracic outlet syndrome (TOS) can feel overwhelming and isolating. The persistent pain, numbness, and weakness in your arms and hands may have disrupted your daily activities, work performance, and quality of life. In this guide, you will find a clear, medically accurate explanation of your condition and the treatment options available to you.
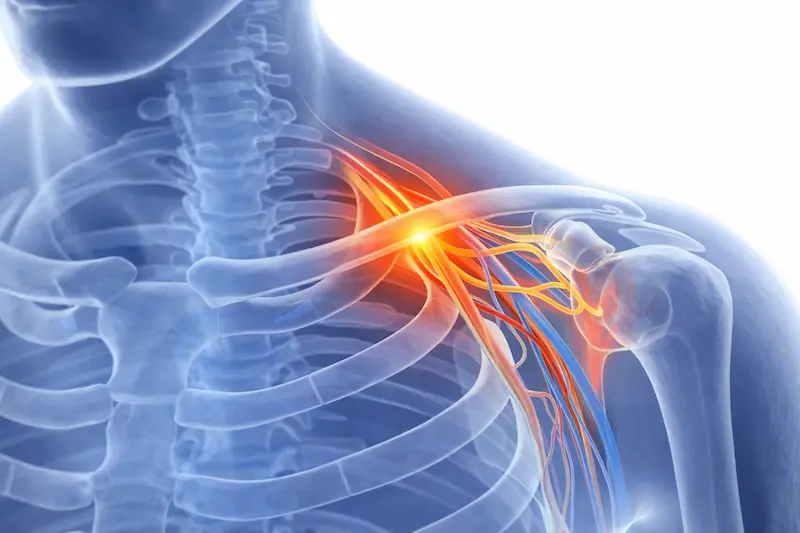
Thoracic outlet syndrome is a complex condition that occurs when blood vessels or nerves (neurovascular structures) in the thoracic outlet—the narrow space between your collarbone and first rib—are compressed or irritated. This compression can cause a variety of symptoms that significantly impact your daily life, from simple tasks like typing at a computer to more demanding activities like lifting objects or playing sports.
The thoracic outlet serves as a crucial passageway for important structures traveling from your neck to your arm, including the brachial plexus nerve (a network of nerves), subclavian artery and vein, and surrounding muscles (mainly the anterior scalene muscle). When this space narrows due to various factors, the resulting compression can lead to debilitating upper-extremity symptoms characteristic of TOS.
Thoracic outlet syndrome manifests in three distinct forms, each requiring a tailored approach to treatment:
Neurogenic TOS is the most common form, accounting for approximately 95% of cases. This type occurs when the brachial plexus compression occurs, typically between the anterior and middle scalene muscles or at the level of the first rib. Patients with neurogenic TOS often experience:
The pain associated with neurogenic TOS can be particularly distressing because it often occurs during routine activities. Many patients describe feeling helpless when sources of significant discomfort become simple tasks, such as reaching for items on a shelf or sleeping in certain positions.

Arterial TOS is the rarest but most serious form of the condition, occurring when the subclavian artery becomes compressed. This type often results from anatomical abnormalities such as cervical ribs or abnormal first ribs. Symptoms of arterial TOS include:

Venous TOS, also known as Paget-Schroetter syndrome or “effort thrombosis,” occurs when the subclavian vein becomes compressed, often leading to blood clot formation. This type typically affects young, athletic individuals who perform repetitive overhead activities. Symptoms include:
Venous TOS constitutes a medical emergency requiring immediate thoracic outlet syndrome treatment to prevent potentially life-threatening complications such as pulmonary embolism.
Not sure which type applies to you? A specialist can help clarify.
They can vary significantly between individuals and may develop gradually over time or appear suddenly following an injury or change in activity level.
Many patients initially dismiss early TOS symptoms as temporary discomfort from poor posture or overuse. However, recognising these early signs can lead to earlier intervention and better outcomes:
Intermittent numbness or tingling in the arms or hands, particularly at night
Occasional sharp or shooting pains from the neck down the arm
Fatigue in the arms during activities that weren’t previously challenging
Sensitivity to cold in the hands and fingers
Subtle changes in grip strength or dexterity
As the condition advances, symptoms typically become more persistent and severe:
Constant aching or burning pain in the neck, shoulder, and arm
Frequent numbness and tingling that interferes with daily activities
Noticeable weakness in the affected arm
Difficulty performing overhead activities
Sleep disruption due to pain and numbness
Changes in skin color or temperature in the affected hand
If these symptoms feel familiar, the next step is understanding the cause.
Thoracic outlet syndrome can develop due to various anatomical, traumatic, or repetitive stress factors. Understanding these causes can help in both prevention and treatment planning.
Some individuals are born with anatomical variations that predispose them to developing TOS:
Trauma to the neck and shoulder region can trigger the development of TOS by causing inflammation, muscle spasm, or scar tissue formation:
Certain occupations and lifestyle factors increase the risk of developing TOS:
Several other factors can contribute to the development or exacerbation of TOS:
Identifying the underlying cause is the first step toward accurate diagnosis and effective treatment.
Accurate diagnosis of thoracic outlet syndrome requires a comprehensive evaluation by an experienced thoracic outlet syndrome specialist. The diagnostic process can be challenging because TOS symptoms can mimic other conditions, and there is no single definitive test for the condition.
While no single imaging study can definitively diagnose TOS, several tests can provide valuable information:
An experienced thoracic surgeon will also consider other conditions that can mimic TOS symptoms:
includes several specialised tests designed to reproduce your symptoms and assess the function of nerves and blood vessels in the thoracic outlet region:

Clinicians may recommend additional tests based on your specific symptoms:
Because no single test can confirm TOS, expert evaluation is essential.
Accurate diagnosis of thoracic outlet syndrome requires a comprehensive evaluation by an experienced thoracic outlet syndrome specialist. The diagnostic process can be challenging because TOS symptoms can mimic other conditions, and there is no single definitive test for the condition.
While no single imaging study can definitively diagnose TOS, several tests can provide valuable information:
An experienced thoracic surgeon will also consider other conditions that can mimic TOS symptoms:
Clinicians may recommend additional tests based on your specific symptoms:
includes several specialised tests designed to reproduce your symptoms and assess the function of nerves and blood vessels in the thoracic outlet region:
Because no single test can confirm TOS, expert evaluation is essential.

Physical therapy forms the cornerstone of conservative TOS treatment. A skilled physical therapist will develop a personalised program addressing your specific symptoms and functional limitations:
Activity Modification
While medications alone rarely cure TOS, they can provide valuable symptom relief during the healing process:


Targeted injection therapy can provide significant symptom relief and diagnostic information:
If conservative treatment does not provide sufficient relief after several months, surgical options may be considered.
Clinicians may recommend surgical intervention when conservative treatment fails to provide adequate symptom relief after 3–6 months of consistent therapy. As a thoracic outlet syndrome surgeon, I understand that the decision to proceed with surgery can feel overwhelming. However, for appropriately selected patients, surgical treatment can provide excellent long-term outcomes and dramatic improvement in quality of life. There are several surgical options, and I will discuss them below.
Clinicians typically recommend surgery when:
Surgeons perform the first rib resection as the most common surgical procedure for TOS, and can perform it through several approaches:
Supraclavicular Approach. This approach involves an incision above the collarbone:
Infraclavicular Approach. Rarely used as a primary approach, but may be necessary in specific situations:
When a cervical rib is present and contributing to symptoms, surgical removal is often necessary. Surgeons typically perform this procedure via a supraclavicular approach and may combine it with first-rib resection for optimal decompression.
Patients with arterial or venous TOS may require additional vascular procedures, which a specialist in vascular surgery performs.
Scalenectomy (removal of scalene muscles) or scalenotomy (division of scalene muscles) may be performed alone or in combination with rib resection:
Surgical treatment is always individualised and based on careful clinical evaluation.
Understanding each step can help you feel more confident and prepared.
Most TOS surgeries are performed under general anaesthesia
Typical duration: 1–3 hours
Depends on individual anatomy and complexity
The goal of surgery is to relieve compression while preserving surrounding structures.
Following surgery, clinicians will monitor you in the recovery area:
Pain management with appropriate medications
Monitoring of arm circulation and neurological function
Gradual mobilisation as tolerated
Most patients can go home the same day or after an overnight stay
Recovery is a gradual, structured process guided by your care team.
The initial recovery period focuses on wound healing and pain management.
Pain management. You’ll receive a comprehensive pain management plan that may include:
Prescription pain medications for the first few days
Anti-inflammatory medications to reduce swelling
Ice therapy for localised pain relief
Gentle positioning techniques to minimise discomfort
Activity restrictions. Initial limitations help protect the healing tissues:
Avoiding lifting more than 5-10 pounds
Limiting overhead arm activities
No driving while taking prescription pain medications
Gentle range of motion exercises as directed
As initial healing progresses, you’ll gradually increase your activity level.
Physical therapy initiation. Most patients begin formal physical therapy 1-2 weeks after surgery:
Gentle range of motion exercises to prevent stiffness
Progressive strengthening of surrounding muscles
Scar tissue mobilisation techniques
Gradual return to functional activities
Work considerations. Return to work depends on your occupation:
Desk workers may return in 1-2 weeks with modifications
Manual laborers may require 6-8 weeks or longer
Activity progression. Gradual increase in daily activities:
Lifting restrictions slowly increase to 15-20 pounds
Driving may resume when you’re no longer taking pain medications
Light recreational activities may be permitted
Overhead activities remain restricted
Understanding realistic expectations for your thoracic outlet syndrome treatment can help you make informed decisions and maintain appropriate hope throughout your recovery journey.
Conservative treatment can be highly effective when properly implemented:
50-80% of patients experience significant symptom improvement with comprehensive conservative treatment
Clinicians see the best results in patients with mild to moderate symptoms and good compliance with therapy
Earlier intervention typically leads to better outcomes
Some patients may require periodic “tune-up” therapy sessions for maintenance

When performed by an experienced thoracic outlet syndrome surgeon, surgical treatment provides excellent results:
Overall success rates:
85-95% of patients experience good to excellent results
Neurogenic TOS typically has the best surgical outcomes
Arterial and venous TOS may require additional procedures, but generally have good outcomes
Patient satisfaction rates are typically very high
Symptom resolution:
Pain relief is often dramatic and immediate in many patients
Numbness and tingling may take several months to resolve fully
Strength typically returns gradually over 3-6 months
Most patients can return to their previous activity level
Factors affecting outcomes:
Earlier surgical intervention generally leads to better results
Patients with isolated neurogenic TOS tend to have better outcomes
Compliance with post-operative rehabilitation is crucial
Pre-existing nerve damage may limit recovery potential
Thoracic outlet syndrome is a treatable condition that, while complex, responds well to appropriate care from experienced specialists. Whether your treatment involves conservative management or surgical intervention, the goal remains the same: helping you return to a comfortable, active lifestyle free from the limitations imposed by TOS symptoms.
If you’re ready to take the next step in addressing your thoracic outlet syndrome, I encourage you to seek consultation with a qualified specialist. With proper treatment and dedication to your recovery, you can look forward to a future free from the pain and limitations of TOS. Your path to recovery starts with that first step— reaching out for the specialised care you deserve. Don’t let thoracic outlet syndrome continue to control your life when effective treatment options are available to help you reclaim your comfort and functionality.
Contact me today to schedule your consultation. Your journey to better health starts with a single phone call.
Take the first step towards expert thoracic care. Dr. Scarci's minimally invasive surgical techniques offer the best chance for successful outcomes with faster recovery times.
London, UK
Multiple clinic locations available
24/7 emergency support available