
Key Takeaways
- Understanding pneumothorax reduces fear and empowers decisions – Learning about collapsed lung types, causes, and symptoms helps patients recognize when to seek care and what to expect
- Multiple treatment options exist from conservative to surgical – Treatment ranges from careful observation for small cases to minimally invasive VATS surgery, tailored to individual circumstances
- Recovery is typically faster and easier than patients expect – Modern techniques enable same-day discharge in many cases, with most patients returning to normal activities within weeks
- Prevention strategies significantly reduce recurrence risk – Pleurodesis procedures offer over 95% success rates, while lifestyle modifications help minimize future pneumothorax episodes
- Comprehensive care addresses both medical and emotional needs – Expert teams provide not just technical treatment but also support for anxiety, family concerns, and quality of life restoration
Finding Comfort in Knowledge – You’re Not Walking This Path Alone
When you first hear the words “collapsed lung” or “pneumothorax,” you might feel confused or even scared. I understand that fear, that moment of uncertainty when everything familiar suddenly feels fragile, the numerous commitments in the diary, the booked holiday, that long-awaited dinner with friends. But here’s what I want you to know from the very beginning: this is a condition that can be easily fixed, and you can get back to normal very quickly.
As someone who has dedicated years to helping patients navigate this exact journey, I’ve witnessed countless individuals move from that initial moment of diagnosis to complete recovery and renewed confidence in their health. The path forward may feel uncertain right now, but with the proper pneumothorax treatment, expert care, and your own resilience, the overwhelming majority of people not only recover fully but go on to live completely unrestricted lives.
Understanding Your Diagnosis
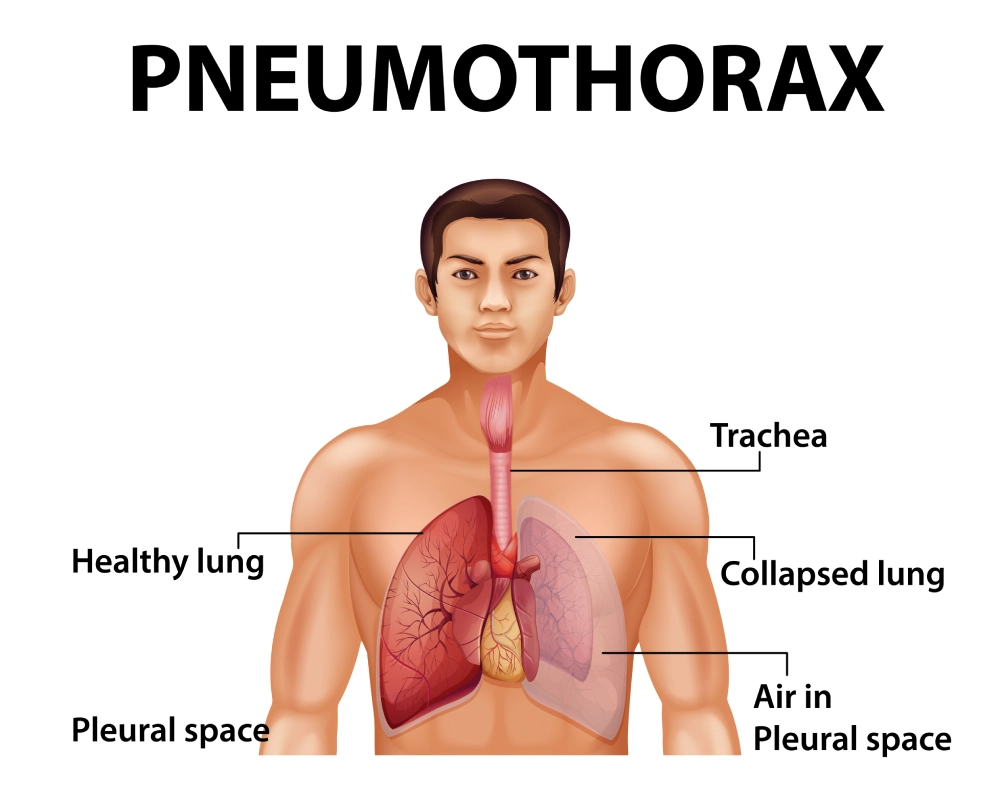
Pneumothorax or punctured lung might sound intimidating, but let’s break it down into understandable terms. Simply put, it occurs when air accumulates in the space between your lung and chest wall, causing the lung to partially or fully collapse. While this sounds frightening, it’s essential to know that modern pneumothorax treatment has transformed what was once a serious condition into something highly manageable with excellent outcomes.
Think of your lungs like balloons inside a box (your chest cavity). Usually, these balloons stay inflated because of the pressure balance around them. When a pneumothorax occurs, air enters the space around the balloon, causing it to deflate. The good news? Just like a balloon can be reinflated, your lung can return to normal function with appropriate specialist pneumothorax treatment.
Types of Pneumothorax – Understanding Your Unique Situation
Primary Spontaneous Pneumothorax: When Healthy Lungs Need Help
Sarah, a 26-year-old yoga instructor from Surrey, was in the middle of teaching a morning class when she felt a sudden, sharp pain in her chest. “I’m healthy, I exercise daily, I don’t smoke,” she told me during our first consultation. “How could this happen to me?”
Sarah’s story represents what we call primary spontaneous pneumothorax – a condition that affects healthy individuals without underlying lung disease. It often occurs in tall, thin young adults and can have a genetic component. If you’re experiencing this type, please know that outcomes are typically excellent, especially with minimally invasive pneumothorax surgery treatment.
“The hardest part was the uncertainty,” Sarah shared six months after her VATS pneumothorax surgery. “But once I understood what was happening and had a clear treatment plan, I felt so much more in control. I’m back to teaching full-time now, and I actually feel more confident about my health than before.”
Sometimes, we simply cannot identify a specific trigger for primary spontaneous pneumothorax, which we term idiopathic pneumothorax. This doesn’t reflect any fundamental weakness in your body – it’s simply how your system responded to a particular set of circumstances that aligned in an unfortunate way.
Secondary Spontaneous Pneumothorax: Managing Complex Conditions with Expertise

David, a 58-year-old teacher with COPD, experienced his first secondary spontaneous pneumothorax episode during a particularly stressful week at work. “I knew my lungs weren’t perfect because of the COPD, but I was managing well with my medications,” he explained. “When this happened, I worried that everything was falling apart.”
Secondary spontaneous pneumothorax occurs in patients with existing lung conditions such as chronic obstructive pulmonary disease (COPD), cystic fibrosis, or other pulmonary diseases. If you have underlying lung conditions, please don’t feel discouraged – specialised pneumothorax treatment tailored to your specific needs offers excellent outcomes even in complex cases.
David’s journey required a coordinated approach between his respiratory specialist and the surgical team. “The team approach gave me such confidence,” he said. “They didn’t just treat the collapsed lung; they helped me understand how to better manage my overall lung health. I feel more secure about my future now than I did before this happened.”
Traumatic Pneumothorax: Healing After Unexpected Events
Mark, a 34-year-old father of two, experienced traumatic pneumothorax during a weekend cycling accident. “One moment I was enjoying a beautiful morning ride, the next I was in the emergency room struggling to breathe,” he recalled. “The fear wasn’t just for myself – I kept thinking about my children needing their dad to be okay.”
Trauma-related pneumothorax from accidents, injuries, or sometimes from medical procedures can feel particularly unsettling because it comes so unexpectedly. But here’s what I want you to know: outcomes for traumatic pneumothorax or tension pneumothorax are often excellent when treated promptly by experienced specialists.
“The emergency medicine team explained everything as they worked,” Mark shared. “Even in that scary moment, their calm expertise helped me feel like I was in capable hands. Six weeks later, I was back on my bike, and my family had their active dad back.”
Very rarely is it possible to develop bilateral pneumothorax. This is a very serious situation that could deteriorate quickly.
Recognising the Signs – Trusting Your Body’s Wisdom
Understanding pneumothorax symptoms empowers you to seek timely care, but remember – your instincts matter too. Many patients tell me, “I knew something wasn’t right,” even before they could articulate specific symptoms.
The primary symptoms to be aware of:
- Sudden chest pain that feels sharp or stabbing, typically on one side of your chest. This isn’t the gradual ache you might feel after exercise – it often comes on suddenly and may worsen when you take deep breaths.
- Shortness of breath that may start mild but can progressively worsen. You might notice you can’t catch your breath the way you normally do, or that activities that usually feel easy now leave you winded.
- Rapid heartbeat and feelings of anxiety are your body’s natural response to the breathing difficulties you’re experiencing.
Lisa, a 29-year-old marketing manager, described her symptoms this way: “I was sitting at my desk when I felt this sudden pain in my left chest. At first, I thought maybe I’d slept wrong or pulled something. But then I noticed I was having trouble taking deep breaths, and my heart was racing. Something inside me said, ‘This isn’t normal,’ and I trusted that feeling.”
When to Seek Immediate Help – Your Safety Comes First
Please seek emergency pneumothorax treatment immediately if you experience:
- Severe shortness of breath that worsens rapidly
- Chest pain that doesn’t improve with rest
- Feeling like you can’t get enough air despite trying to breathe deeply
- Bluish tint to your lips or fingertips
- Rapid heart rate combined with chest pain
- Feeling faint or dizzy, along with breathing difficulties
“I almost talked myself out of going to the hospital,” shared James, a 31-year-old engineer. “I kept thinking, ‘Maybe I’m overreacting.’ But my wife insisted, and I’m so grateful she did. The medical team told me that coming in when I did prevented the situation from becoming much more serious.”
Remember: you know your body better than anyone else. If something feels significantly different or wrong, trust that instinct. Emergency pneumothorax treatment is designed precisely for these situations, and seeking help quickly often leads to better outcomes and shorter recovery times.
Understanding the Causes – Finding Peace Through Knowledge
Why This Happened to You
One of the most common questions I hear is, “Why did this happen to me?” The need to understand is natural and completely valid. While we can’t always identify a specific trigger, understanding potential causes can help you feel more in control and make informed decisions about the prevention of pneumothorax in the future.
Common causes include:
- Small air sacs (blebs) rupture on the lung surface – these are like tiny bubbles that can form on healthy lungs and occasionally pop, much like a soap bubble.
- Chest trauma from accidents, falls, or injuries – sometimes the chest wall or ribs can be impacted in ways that affect the pleural space.
Complications from medical procedure – occasionally, procedures like biopsies or central line placements can inadvertently cause an iatrogenic pneumothorax. This doesn’t represent a medical error; it’s a known possible complication that medical teams are prepared to handle.
Underlying lung disease, such as asthma, COPD, or infections, can create conditions that make pneumothorax more likely.
Spontaneous pneumothoraces in otherwise healthy individuals – sometimes it simply happens without an identifiable cause.
Special Considerations: When Pneumothorax Has Unique Patterns
Catamenial Pneumothorax: Understanding a Woman’s Health Connection
Emma, a 32-year-old nurse, noticed a disturbing pattern over several months. “I kept having these episodes of chest pain and breathing problems around the same time each month,” she explained. “Three different emergency room visits later, someone finally connected the dots to my menstrual cycle.”
Emma was experiencing catamenial pneumothorax, a rare condition that affects women and typically occurs around menstruation due to endometriosis involving the pleura. If you’re a woman experiencing recurrent pneumothorax that seems to follow a monthly pattern, this specialised condition requires evaluation from a specialist experienced in both hormonal and surgical aspects of care.
“Finding a doctor who really understood this condition changed everything,” Emma said after her successful treatment. “It wasn’t just about treating the lung problem – it was about understanding how my body’s complex systems were interconnected. I finally felt heard and properly cared for.”
Genetic Factors: When Pneumothorax Runs in Families
Tom, a 28-year-old software developer, felt worried when he learned his uncle and cousin had both experienced pneumothorax. “When it happened to me too, I started wondering if I was destined for repeated episodes,” he shared.
Several genetic conditions can predispose individuals to pneumothorax:
- Marfan syndrome, which affects connective tissues throughout the body
- Birt-Hogg-Dubé syndrome, which causes small cysts to form in the lungs
- Lymphangioleiomyomatosis (LAM), which primarily affects women of childbearing age
If you have a genetic condition that increases pneumothorax risk, please don’t feel discouraged. Specialised pneumothorax treatment programs are available that offer personalised care addressing your unique genetic considerations while providing excellent outcomes.
“Understanding the genetic component actually gave me peace of mind,” Tom explained after his preventive pneumothorax surgery. “Instead of worrying about when it might happen again, I took control and had the pleurodesis procedure. Now I know I’ve done everything possible to prevent future episodes.”
Lifestyle Factors: Choices That Impact Your Risk

The Impact of Smoking
I need to address smoking directly because it significantly increases pneumothorax risk, but I want to do so with compassion rather than judgment. If you smoke, you’re not being lectured – you’re being given information that could protect your health.
Rachel, a 35-year-old teacher, had been smoking for fifteen years when she experienced her first pneumothorax. “I knew smoking was bad for my lungs, but I never connected it to something like a collapsed lung,” she said. “This experience was the wake-up call I needed.”
Smoking increases pneumothorax risk by weakening lung tissue and creating conditions that make air leaks more likely. If you smoke and have experienced pneumothorax, quitting is one of the most powerful steps you can take to prevent future episodes.
“Quitting wasn’t easy, but having a concrete health scare made the motivation real,” Rachel shared six months later. “My care team connected me with excellent cessation resources, and I haven’t had another episode since I quit.”
Occupational and Recreational Considerations
Some activities and occupations carry higher pneumothorax risks:
- Scuba diving due to pressure changes
- Aviation, both as a pilot and a frequent flyer
- High-altitude activities like mountain climbing
- Contact sports with risk of chest trauma
If you participate in these activities, this doesn’t mean you need to stop living your life. It means working with a thoracic surgeon to understand your individual risk profile and potentially considering preventive pneumothorax surgery if you’re at higher risk for recurrence.
Captain Williams, an airline pilot who experienced pneumothorax, chose to have VATS pneumothorax surgery with pleurodesis to ensure he could continue his career without medical restrictions. “My livelihood depended on having absolutely reliable lungs,” he explained. “The surgery gave me that confidence and allowed me to return to flying without limitations.”
Treatment Options – Your Path to Healing
A Personalised Approach to Your Recovery
The beauty of modern pneumothorax treatment lies in how it can be tailored specifically to your unique situation. No two patients are exactly alike, and your treatment for pneumothorax should reflect your individual needs, health status, lifestyle, and personal preferences.
When developing your personalised pneumothorax care plan, we consider multiple factors:
- Size and severity of your pneumothorax
- Your symptoms and how they’re affecting your daily life
- Previous episodes and your personal medical history
- Underlying health conditions that might influence treatment choices
- Your age, fitness level, and lifestyle factors
- Your personal preferences and concerns about different treatment options
- Your occupation and any specific requirements for lung function
Conservative Management – When Gentle Care is Enough

For small pneumothorax cases (typically less than 20% lung collapse) without significant symptoms, we often begin with careful observation. This approach might feel like “doing nothing,” but it’s actually a sophisticated medical strategy based on your body’s remarkable ability to heal itself.
Michael, a 27-year-old accountant, was anxious when told his small pneumothorax would be managed conservatively. “I wanted them to do something,” he said. “But they explained that my body was already working to fix the problem, and they were there to support that process.”
Conservative management includes:
- Regular monitoring with chest X-rays to track healing progress
- Oxygen therapy to help your body absorb the trapped air more quickly
- Close observation for any changes in your condition
- Clear guidelines on what symptoms should prompt immediate medical attention
- Regular follow-up appointments with your pneumothorax specialist
“By the end of the first week, I could see the improvement on the X-rays,” Michael shared. “It was actually empowering to watch my body heal itself with expert medical support. I felt like an active participant in my recovery rather than a passive patient.”
Minimally Invasive Interventions – Gentle but Effective
Needle Aspiration – Quick Relief When You Need It
Needle aspiration is often the first intervention for primary spontaneous pneumothorax in appropriate patients. This procedure involves inserting a small needle into the pleural space to remove trapped air, usually providing almost immediate relief from symptoms.
Jennifer, a 24-year-old graphic designer, underwent needle aspiration for her first pneumothorax episode. “I was terrified of the needle, but the local anaesthetic made it completely tolerable,” she recalled. “The relief was almost instant – I could suddenly take deep breaths again.”
Benefits of needle aspiration:
- Quick procedure performed with local anaesthetic
- Minimal discomfort compared to other interventions
- Often, an outpatient procedure allows you to go home the same day
- Immediate symptom relief in successful cases
- Low complication rate when performed by experienced specialists
“What surprised me most was how normal I felt afterward,” Jennifer said. “I expected to feel weak or fragile, but I actually felt stronger knowing that I’d been through this and come out fine.”
Chest Tube or Chest Drain Insertion – Effective Drainage for Larger Cases
Chest tube drainage involves placing a flexible tube into the pleural cavity to continuously drain air and allow lung re-expansion. While the idea of having a tube in your chest might sound intimidating, modern techniques make this a much more comfortable experience than many patients anticipate.
Robert, a 45-year-old construction manager, needed a thoracostomy tube for his large pneumothorax. “I’ll be honest – the idea scared me,” he admitted. “But the medical team explained everything step by step, and the experience was much less traumatic than I’d imagined.”
What to expect with chest tube insertion:
- Local anaesthetic ensures the insertion is not painful
- Continuous drainage allows gradual, comfortable lung re-expansion
- Expert nursing care with regular monitoring and support
- Effective pain management to keep you comfortable throughout
- Mobility encouraged – you can walk around with the tube in place
- Typical duration of 1-3 days until removal
“The nurses were incredible,” Robert shared. “They helped me understand what was normal and what to expect. By the second day, I was walking the halls and felt like myself again. When they removed the tube, it was such a relief to know my lung was fully expanded and healthy.”
Advanced Lung Surgery – When Definitive Surgical Treatment is Needed

VATS (Video Assisted Thoracoscopic Surgery) – The Gold Standard
Minimally invasive pneumothorax surgery using VATS represents the pinnacle of modern pneumothorax treatment. As a surgeon who specialises in these techniques, I can assure you that this approach offers excellent outcomes while minimising trauma to your body.
Sarah, a 30-year-old teacher who had experienced two pneumothorax episodes, chose VATS surgery to prevent future occurrences. “I couldn’t live with the uncertainty,” she explained. “Every time I felt any chest sensation, I worried it was happening again. I needed the peace of mind that surgery could provide.”
VATS advantages:
- One small incision
- High-definition camera providing magnified views of the entire pleural space
- Precise surgical repair with minimal tissue disruption
- Shorter hospital stays compared to traditional open surgery
- Faster recovery and quicker return to normal activities
- Significantly reduced post-operative pain
- Minimal scarring that’s barely visible once healed
During VATS surgery, we can:
- Identify and repair the exact source of your pneumothorax
- Remove problematic blebs or bullae that could cause future episodes
- Perform pleurodesis to prevent recurrence
- Address any underlying abnormalities we discover
“The recovery was so much easier than I expected,” Sarah shared three months post-surgery. “I was back at work within two weeks and felt completely normal within a month. Most importantly, I haven’t worried about pneumothorax since. It’s such a relief to have my life back.”
Open Thoracotomy – When Complex Cases Require Direct Access (This is very rare)
Occasionally, open thoracotomy may be necessary for complex cases or emergencies. While this involves a larger incision, modern surgical techniques and pain management make even these procedures much more tolerable than in the past.
David, a 52-year-old with multiple previous episodes and complex scarring, required open surgery. “I was nervous about the bigger surgery, but my surgeon explained why it was the best approach for my particular situation,” he said. “The care I received was outstanding, and the results have been excellent.”
Open thoracotomy may be recommended for:
- Complex recurrent cases with extensive internal scarring
- Emergencies requiring immediate surgical access
- Large or complicated pneumothorax with multiple problem areas
- Previous surgical attempts that weren’t entirely successful
- Specific anatomical considerations that make minimally invasive techniques challenging
Pleurodesis – Long-term Prevention You Can Count On
Pleurodesis is a procedure that creates controlled adhesions between your lung and chest wall, effectively eliminating the space where air can accumulate and cause future pneumothorax. Think of it as creating permanent “glue” between the lung and chest wall.
Chemical Pleurodesis – Highly Effective Prevention
Talc pleurodesis involves introducing medical-grade talc powder that causes controlled inflammation and scarring, creating permanent adhesions.
Mark, a 35-year-old pilot, chose chemical pleurodesis as part of his VATS surgery. “My career depends on having completely reliable lungs,” he explained. “The chemical pleurodesis gave me a 95% guarantee that I’d never have another episode. For me, those odds were worth it.”
Advantages of chemical pleurodesis:
- Extremely high success rate (over 95% in preventing recurrence)
- Can be performed during surgery or through a chest tube
- Well-tolerated by the vast majority of patients
- Provides lifelong protection against future pneumothorax
- No significant long-term side effects for most patients
Mechanical Pleurodesis – Immediate and Effective
Mechanical pleurodesis involves gently abrading the pleural surfaces during surgery to create adhesions without introducing foreign substances.
Lisa, who was concerned about introducing chemicals into her body, chose mechanical pleurodesis. “I liked the idea of using my body’s own healing response,” she said. “The results have been excellent, and I feel confident knowing it was done naturally.”
Benefits of mechanical pleurodesis:
- Immediate effect – no waiting period for results
- Highly effective in preventing recurrence
- No foreign substances were introduced into your body
- It can be precisely controlled during surgery
- Excellent long-term outcomes
Real-Life Success Stories – Hope Through Experience

Emma’s Journey: From Fear to Confidence
Emma, a 28-year-old veterinarian from Kent, experienced her first pneumothorax during emergency surgery on a dog. “The irony wasn’t lost on me,” she laughed during our follow-up appointment. “I was trying to save an animal’s life when my own lung collapsed.”
Initial Challenge: Emma’s pneumothorax occurred at the worst possible time – during a critical veterinary procedure. “I felt this sudden pain, but tried to continue the surgery. My assistant noticed I was struggling to breathe and insisted I sit down.”
Treatment Journey: After emergency chest tube insertion, Emma opted for VATS pneumothorax surgery with pleurodesis. “As a veterinarian, I understood the medical aspects, but experiencing it as a patient was completely different. The emotional support from the medical team was just as important as the technical expertise.”
Life-Changing Results: Eighteen months later, Emma has returned to full practice without restrictions. “I perform long surgeries without any worry about my lungs. The pneumothorax surgery didn’t just fix the immediate problem – it gave me complete confidence in my body again. I’m actually a better veterinarian now because I understand what my clients go through when their pets need surgery.”
James’s Athletic Recovery: Getting Back in the Game
James, a 26-year-old semi-professional rugby player from Manchester, faced the possibility that his sporting career might be over after his second pneumothorax in six months.
The Athletic Challenge: “Rugby is my passion and my livelihood,” James explained. “When the second episode happened during training, I thought my career was finished. The fear of it happening during a match was overwhelming.”
Specialised Sports Medicine Approach: James worked with our team to develop a pneumothorax treatment plan specifically designed for athletes. “They understood that getting back to sport wasn’t just about physical recovery – it was about psychological confidence too.”
Triumphant Return: After minimally invasive pneumothorax surgery with pleurodesis, James returned to competitive rugby within three months. “The surgery was the best decision I ever made. Not only have I returned to playing, but I play with more confidence than before because I know this won’t happen again. Last month, we won the regional championship, and I scored the winning try.”
Margaret’s Mature Perspective: Health After 60
Margaret, a 64-year-old retired teacher from Brighton, developed secondary pneumothorax related to mild COPD she’d been managing for years.
Unique Concerns: “At my age, any surgery feels more risky,” Margaret shared. “I was worried about recovery time and whether the benefits would outweigh the risks.”
Comprehensive Care Approach: Margaret’s treatment involved careful coordination between respiratory medicine and thoracic surgery. “The team took extra time to explain everything and ensure I was comfortable with each decision. They never made me feel like my concerns weren’t valid because of my age.”
Renewed Vitality: Six months after her pneumothorax surgery, Margaret has better lung function than before her pneumothorax. “The surgery not only fixed the collapsed lung but also improved my overall COPD management. I’m more active now than I was before this happened. I’ve started volunteering at the local library and even took up watercolor painting – activities I’d avoided because of breathing concerns.”
Thomas’s Professional Success: Executive Leadership Under Pressure
Thomas, a 42-year-old CEO of a London-based technology company, experienced recurrent pneumothorax during the most demanding period of his career.
High-Stakes Challenge: “I was leading our company through a major acquisition when the second episode occurred during a crucial board meeting,” Thomas recalled. “The stress of wondering when it might happen again was affecting my ability to lead effectively.”
Executive-Level Care: Thomas chose a private care pathway that fit his professional commitments. “The concierge-level service meant I could continue working around my treatment schedule. Video calls from my hospital room, same-day discharge – it was all arranged to support my business needs.”
Leadership Restoration: Thomas returned to full executive function within two weeks of his VATS pneumothorax surgery. “The procedure was successful, but more importantly, it restored my confidence as a leader. I no longer worry about health issues during high-pressure situations. Our acquisition was completed successfully, and the company has grown 40% since then. I credit part of that success to having my health completely sorted out.”
Rachel’s Family Focus: Motherhood Without Limits
Rachel, a 33-year-old mother of three young children from Surrey, experienced pneumothorax while chasing her toddler in the park.
Maternal Concerns: “My first thought wasn’t about me – it was about my children. What if this happened when I was alone with them? What if I couldn’t take care of them?” Rachel’s fear centered on her role as primary caregiver.
Family-Centered Treatment: Rachel’s pneumothorax treatment plan was designed around her family obligations. “The medical team understood that I wasn’t just a patient – I was a mom. They arranged weekend surgery so my husband could be home, and provided detailed instructions for childcare during recovery.”
Complete Family Life Restoration: Three months post-surgery, Rachel has returned to all activities with her children. “I run with them, play soccer in the garden, carry them when they’re tired – everything I did before and more. The kids don’t even remember when mommy had to rest. Most importantly, I don’t worry about having another episode while I’m caring for them. That peace of mind has made me a more relaxed, present parent.”
Your Recovery Journey – Healing with Confidence

Setting Realistic Expectations
Recovery from pneumothorax surgery has been revolutionised by modern minimally invasive techniques. While I want to be honest about what to expect, I also want to reassure you that most patients are pleasantly surprised by how well they feel throughout their recovery journey.
The First 48 Hours – Professional Care When You Need It Most
Hospital experience designed for comfort:
Your recovery begins in a private room with nursing staff specifically trained in thoracic surgery care. These aren’t just medical professionals – they’re compassionate advocates for your comfort and recovery.
“I was amazed by how attentive everyone was,” shared David, reflecting on his hospital stay. “Every nurse knew my name, understood my concerns, and took time to explain what they were doing. It felt like having a medical family caring for me.”
Pain management that works:
Modern pain management uses multiple approaches to ensure your comfort:
- Pre-emptive pain control that prevents discomfort before it starts
- Patient-controlled analgesia puts you in charge of your comfort level
- Non-medication techniques like positioning and breathing exercises
- Anti-inflammatory medications to reduce surgical site discomfort
“I was worried about pain, but they stayed ahead of it,” explained Jennifer after her VATS pneumothorax surgery. “I never experienced severe discomfort, and by the second day, I was using very little pain medication.”
Family involvement and communication:
Your loved ones receive regular updates throughout your recovery, and visiting is encouraged as soon as you’re ready. Many patients find that having family present actually speeds their recovery by reducing anxiety and providing emotional support.
Week One – Finding Your New Normal
Gentle return to daily activities:
The first week home focuses on gradual increases in activity while allowing your body to heal. Most patients are surprised by how much they can do relatively quickly.
Breathing exercises that empower:
You’ll receive specific breathing exercises designed to optimise your lung expansion and prevent complications. These aren’t just medical necessities – they’re empowering tools that help you actively participate in your recovery.
“The breathing exercises made me feel like I was doing something positive for my healing,” said Mark. “Instead of just waiting to get better, I was actively helping my lungs recover. That sense of control was incredibly important to my mental state.”
Progressive activity guidelines:
- Days 1-3: Rest with gentle walking as tolerated
- Days 4-7: Increased walking, light household activities
- Week 2: Return to work for most desk jobs
- Week 3-4: Driving and normal daily activities
- Week 4+: Full activity clearance based on individual progress
Managing Recovery Challenges with Support

When Healing Feels Slow
Some days will feel better than others, and that’s completely normal. Sarah experienced this during her recovery: “There were days when I felt like I was moving backward instead of forward. My surgeon reminded me that healing isn’t always linear, and that reassurance helped me stay patient with the process.”
Strategies for challenging days:
- Regular communication with your surgical team
- Realistic day-by-day goals rather than focusing on outcomes
- Celebration of small victories, like taking deeper breaths or walking further
- Family and friend support for encouragement
- Professional counselling if anxiety about recovery persists
Emotional Aspects of Recovery
The emotional journey of recovery is often underestimated but incredibly important. Many patients experience a range of feelings during healing.
“I didn’t expect the emotional roller coaster,” admitted Tom. “Some days I felt grateful and optimistic, other days I felt anxious about returning to normal activities. Talking about these feelings with my medical team helped me understand they were normal parts of recovery.”
Common emotions during recovery:
- Relief that the surgery is complete and successful
- Anxiety about returning to full activities
- Gratitude for medical care and family support
- Impatience with the healing timeline
- Confidence as milestones are achieved
Long-Term Success – Living Without Limitations
Return to Full Life Engagement
The goal of pneumothorax surgery isn’t just medical cure – it’s complete restoration of your quality of life. Most patients not only return to their previous activities but often engage more fully because their health anxiety has been resolved.
Captain Williams, the airline pilot, summarised it perfectly: “Before the surgery, I was always listening to my body, worried about every little chest sensation. After recovery, I stopped thinking about my lungs at all – which is exactly how it should be. I’m flying more hours than ever and loving every minute of it.”
Professional and Personal Achievements
Many patients find that resolving their pneumothorax actually opens new possibilities in their lives. When health anxiety is eliminated, energy and focus can be redirected towards personal and professional goals.
Rachel, the mother of three, started a small business from home after her recovery. “Having my health completely sorted out gave me the confidence to take on new challenges. I wasn’t worried about having medical emergencies that would interfere with my business commitments.”
Comprehensive Treatment Options – Your Pathway to the Best Care
Private Care for Pneumothorax – Excellence Without Compromise
Private pneumothorax treatment offers several distinct advantages that can significantly impact your experience and outcomes:
Immediate access to specialist care:
- Same-day consultations when you need urgent evaluation
- No NHS waiting times for treatment or surgery
- Direct access to leading pneumothorax specialists
- Flexible appointment scheduling around your life and work
Personalised, unhurried care:
- Extended consultation times to address all your concerns
- Personalised treatment plans developed specifically for your situation
- Dedicated nursing staff throughout your care journey
- Family involvement in treatment planning and decision-making
State-of-the-art facilities:
- Modern surgical suites with the latest technological advances
- Comfortable private rooms for optimal recovery
- Advanced diagnostic imaging with immediate results
- Comprehensive support services under one roof
Emergency Care – When Every Minute Counts
24/7 emergency pneumothorax treatment ensures that expert care is available exactly when you need it most:
Immediate response capabilities:
- Direct access to pneumothorax surgeons around the clock
- Rapid diagnostic assessment with chest X-ray and CT scanning
- Same-day surgical intervention if required
- Seamless admission to private facilities
- Family notification and support throughout emergency care
Comprehensive emergency services:
- Advanced life support capabilities and critical care medicine
- Expert anaesthesia services are available immediately
- Complete surgical teams on standby
- Post-operative intensive monitoring as needed
- Coordination with your regular medical team
Advanced Pneumothorax Surgery – Technical Excellence with Compassion
Pneumothorax surgery has evolved to offer patients the most advanced techniques with optimal outcomes:
Minimally invasive pneumothorax surgery:
- VATS (Video-Assisted Thoracoscopic Surgery) as the gold standard
- Single-incision techniques for appropriate cases
- Robotic-assisted surgery for complex procedures
- Same-day discharge possible for selected patients
- Immediate management of pneumothorax recurrence