You might expect a thoracic surgeon to always recommend surgery. But alternatives to surgery are often the best path forward.
But here’s a truth more patients need to hear: Some of the best decisions I’ve made were the ones not to operate.
Yes, I love the operating theatre. But I love good outcomes more. And sometimes the best outcome comes from restraint—not intervention.
Let me show you what that looks like in real life.
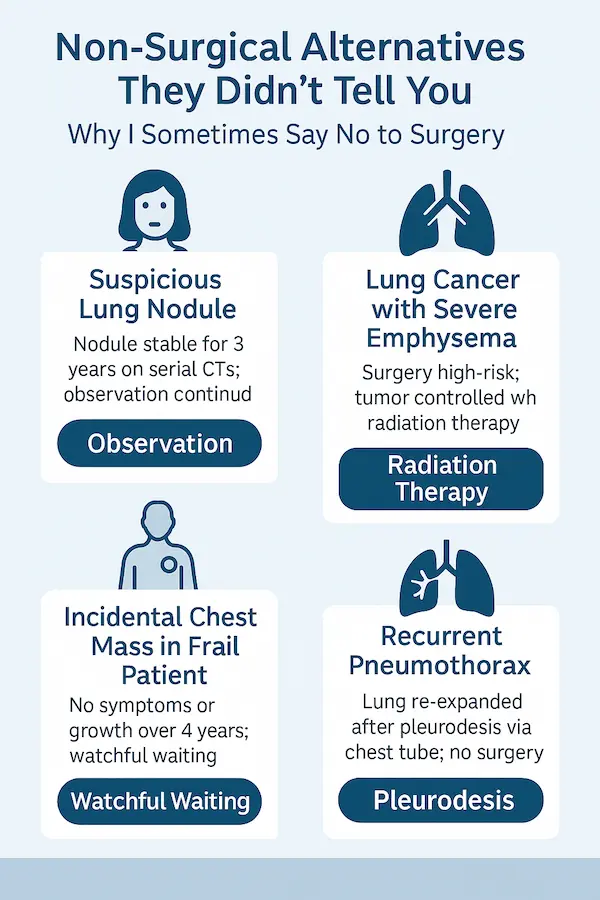
1. The “Suspicious” Lung Nodule That Didn’t Need a Scalpel
Maria, 63, had a 6mm nodule picked up on a CT scan. Her GP was understandably concerned. She was referred urgently and sat in front of me, terrified she had cancer.
We reviewed the imaging. The nodule was smooth-edged, stable in size, and had the classic features of a benign granuloma.
She was ready to book surgery. I said no.
We opted for serial CT scans every 6 months– a proven alternative to surgery for stable nodules. Three years later? It hasn’t changed a bit.
Lesson: Not every shadow needs a knife. Observation is sometimes the most powerful tool.
2. A Patient with Emphysema and Lung Cancer — But the Surgery Would Have Broken Him
Clive, 70, had early-stage lung cancer. A lobectomy might have cured him. But he also had severe COPD, barely walking 50 feet without oxygen.
Could we technically operate? Yes. But he might never come off a ventilator. So we discussed alternatives to surgery.
He underwent stereotactic body radiotherapy (SBRT)—a highly focused radiation treatment. It worked. He kept his independence. And he’s now 2 years post-treatment, cancer-free.
Lesson: Just because we can operate, doesn’t mean we should.
3. An Incidental Chest Mass in a Frail Patient — and the Power of Doing Nothing
Nora, 82, came in with an incidental anterior mediastinal mass. No symptoms. No compression. Just fear.
She was fragile—mild dementia, multiple medications, and already dependent for care. Surgery could’ve easily made everything worse.
We chose watchful waiting– one of the safest alternatives to surgery for frail patients- checking imaging yearly. Four years later, no change. Nora passed away peacefully from unrelated causes. Her chest mass never became an issue.
Lesson: In older patients, the question isn’t just “What is it?”—it’s “Will this thing harm them before something else does?”
4. Recurrent Pneumothorax in a Man with Emphysema — Fixed Without Surgery
Jake, 73, came in with his second pneumothorax. He was thin and terrified of hospitals.
Instead of rushing to VATS surgery, we did pleurodesis through a chest tube—a non-surgical approach to stick the lung to the chest wall.
It worked. He went home in two days. Five years later, he’s still symptom-free.
Lesson: For selected cases, non-operative pleurodesis is effective—and avoids the trauma of surgery.
Why I Sometimes Say No and Suggest Alternatives to Surgery
I became a surgeon to help people—but that doesn’t mean cutting everyone open.
Sometimes my best decision is made in the clinic, not the operating theatre.
Surgery carries risk. Even “routine” procedures have consequences: pain, infection, complications, and changes to quality of life.
When I sit with a patient, I ask:
- What does success look like for you?
- Will this surgery actually make your life better—or just look good on paper? actually make your life better—or just look good on paper?
If the answer is unclear, I pause. We talk. We weigh options together.
Final Word: Surgery Is a Tool, Not a Lifestyle
The best surgeons don’t just know how to operate—they know when not to.
If you ever feel like you’re being rushed to theatre without a clear explanation of alternatives, ask this:
“Doctor, what would you recommend if I were your family?”
If they hesitate to explore non-surgical paths, get a second opinion.
Because the goal isn’t surgery. It’s healing.