When it comes to investigating a chest or lung concern, the most important difference between a CT scan and an MRI is how they see inside your body. A CT scan uses X-rays to create remarkably clear, detailed pictures of lung tissue and bone. An MRI, on the other hand, uses powerful magnets and radio waves and is exceptional at showing soft tissues.
The right scan for you depends entirely on what your specialist needs to assess, as each technology gives us a unique and valuable window into what’s happening in your chest.
Understanding Your Scan Options: CAT Scan vs MRI
If you've ever felt a bit lost trying to make sense of medical imaging, you're certainly not alone. Hearing terms like "CT" or "MRI" can be confusing, especially when you’re already concerned about your health. The first step towards feeling more in control is simply understanding what these scans are and why one might be chosen over the other.
Think of it this way: a CT scan is like rapidly flicking through the pages of a book to get a quick, sharp overview of the whole story. It’s perfect for spotting issues like nodules in the lungs or fractures in the ribs. An MRI is more like studying a single page with a magnifying glass, revealing intricate details in soft tissues like muscles, the heart, or the chest wall that a CT might not pick up.
Core Technology: A Quick Breakdown
The fundamental difference is in the physics. A Computed Tomography (CT or CAT) scan takes a series of X-ray images from many different angles and uses a computer to produce cross-sectional, or ‘slice-like’, pictures of your body. It's incredibly fast and provides excellent clarity for structures like the lungs.
Magnetic Resonance Imaging (MRI) is a completely different beast. It uses a strong magnetic field and radio waves to generate its images, a process that involves no radiation at all. This makes it the gold standard for visualising soft tissues, such as the heart, chest wall, and the areas immediately surrounding the lungs.
A Patient's Story: The Importance of the Right Scan
A patient of mine, a gentleman in his early 70s, came to me after a CT scan found a mass in his lung. The CT was perfect for identifying the tumour, but its location was tricky—right up against his diaphragm. To plan for surgery, I needed to know if the tumour was invading the diaphragm, a detail the CT couldn't clearly show. We used an MRI, which provided a crystal-clear image of the soft tissue, confirming there was a safe margin for a keyhole procedure. You can hear more about his journey in the video below; it’s a perfect example of how CT and MRI work together to create the full picture.
Deciding Between a CT and an MRI
This choice is never arbitrary; it’s a clinical decision driven by your specific symptoms and the exact anatomy we need to examine. This simple decision tree shows the basic principle behind choosing a scan.
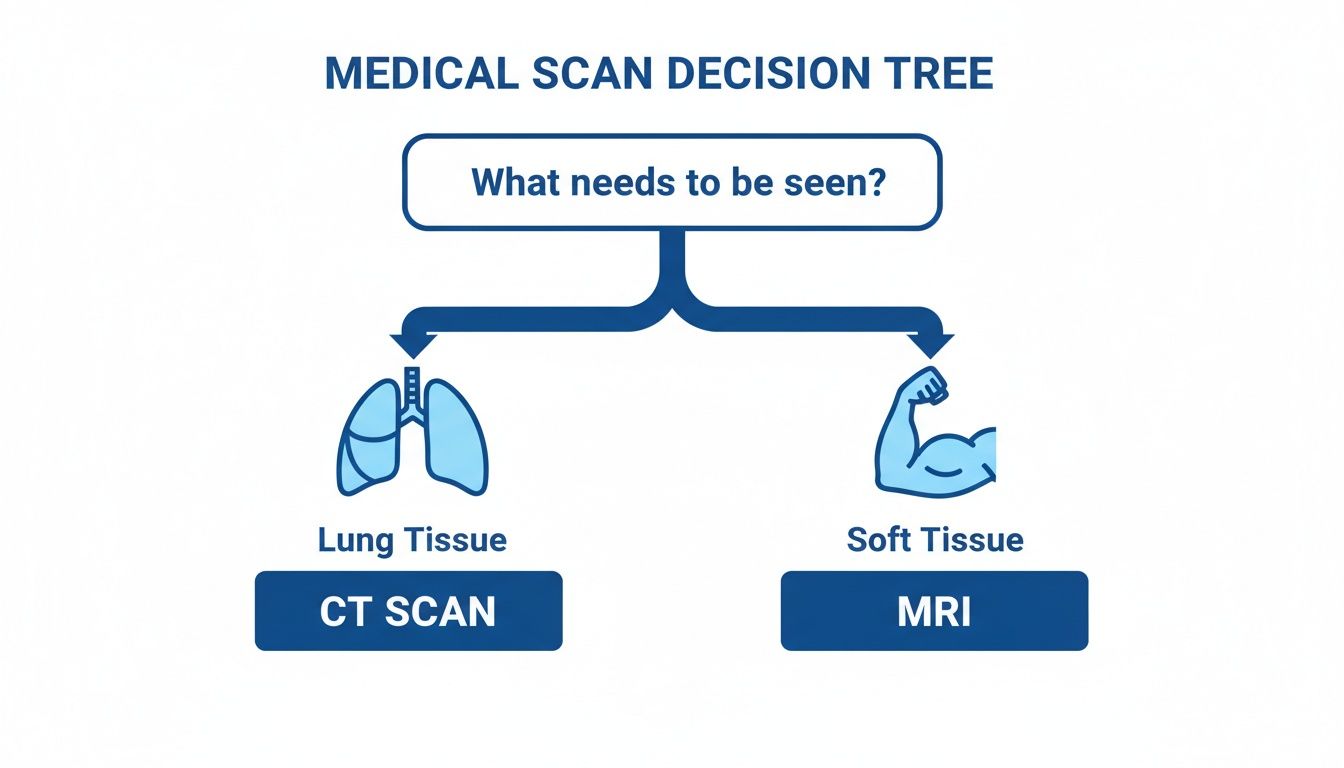
As the guide shows, if the concern is directly related to the lung's structure itself, a CT scan is almost always the first port of call. For detailed soft tissue evaluation, however, an MRI is often preferred. This initial choice sets the stage for your entire diagnostic journey, which is why understanding what happens at a thoracic appointment can help you feel better prepared for what comes next.
Quick Comparison: CT Scan vs MRI for Chest Imaging
For a straightforward summary, this table breaks down the key distinctions between the two scans when used for thoracic conditions.
| Feature | CT (CAT Scan) | MRI |
|---|---|---|
| Technology Used | X-rays and computer processing | Magnets and radio waves |
| Best For | Lung tissue, bone, fast imaging | Soft tissues, organs, chest wall |
| Scan Duration | Very fast (typically 5-10 minutes) | Slower (typically 30-60 minutes) |
| Radiation Exposure | Yes (low, controlled dose) | No |
While both are powerful diagnostic tools, their strengths are in different areas. The speed and lung detail of a CT make it indispensable for many thoracic issues, whereas the safety and soft-tissue clarity of an MRI are vital in other clinical scenarios.
A Patient's Diagnostic Journey Through Thoracic Imaging

Sometimes the best way to understand the difference between a cat scan v mri is to walk through a real-world clinical scenario. Let’s imagine a patient, David, a 65-year-old retired teacher from London who has had a persistent cough for weeks. He initially dismisses it, but his wife eventually convinces him to see his GP.
David’s journey, like many, starts with a standard chest X-ray. It gives a good first look, but the radiologist notices something concerning: a small, hazy area—a nodule—in his right lung. The image lacks the detail needed for a confident diagnosis, leaving everyone with questions and the clear need for a closer look.
To get that clarity, David's GP refers him to a thoracic specialist. The specialist explains that the next essential step is a CT scan, which is widely recognised as the gold standard for imaging the lung parenchyma (the lung tissue itself).
The First Step: A CT Scan
David arrives for his CT scan feeling a bit nervous, which is completely understandable. The radiographer reassures him, explaining that the procedure is both quick and painless. He lies on a table that glides into the centre of a large, doughnut-shaped machine—the gantry of the CT scanner.
He’s asked to hold his breath for just a few seconds at a time as the machine captures the images. The entire process is over in under ten minutes. The result? A series of incredibly detailed, cross-sectional pictures of his chest.
A CT scan gives us an anatomical map of the lungs with breathtaking clarity. For David, it transforms the vague shadow from his X-ray into a sharply defined, 8mm nodule, revealing its precise size, shape, and location. This level of detail is absolutely critical for planning the next steps.
Throughout a patient's diagnostic path, options like virtual doctor visits are becoming more common for discussing initial symptoms or reviewing imaging results. In David's follow-up, it’s clear the CT has provided vital information but has also raised a new question.
When an MRI Complements the CT
The CT scan reveals the nodule is positioned very close to the chest wall. While the CT provides a superb view of the nodule itself, the specialist now needs to know if it's involving the surrounding soft tissues, like the muscles between the ribs. This is precisely where an MRI excels.
An MRI is ordered, not to look at the lung nodule again, but to focus specifically on the chest wall. David finds the MRI machine to be a longer, more enclosed tunnel than the CT scanner. He’s given headphones to help muffle the loud knocking and banging sounds the machine makes.
This scan takes longer, around 45 minutes, and it's crucial for David to stay as still as possible to get sharp images.
- CT Scan’s Role: To precisely identify and characterise the nodule within the airy lung tissue.
- MRI’s Role: To provide superior detail of the soft tissues—the chest wall, muscles, and nerves.
The MRI results bring good news. They show a clean margin between the nodule and the chest wall; it hasn't invaded the surrounding structures. This one piece of information, gained by using the MRI to complement the CT, confirms that David is an ideal candidate for minimally invasive keyhole surgery.
David’s story perfectly illustrates a core principle in the cat scan v mri debate: they aren't competitors, but collaborators. One gives us a swift, detailed map of the lungs, while the other offers an unparalleled look at the soft tissue landscape. Used together, they build the complete diagnostic picture needed to guide surgeons and, most importantly, reassure patients.
How CT and MRI Actually See Inside Your Chest
To get to the heart of the CT versus MRI debate for chest conditions, you have to appreciate what each scan actually shows us. They’re not just different machines; they reveal fundamentally different aspects of your anatomy. Think of them as two distinct visual languages. As thoracic specialists, we need to be fluent in both to understand the full story.
A CT scanner is like a master architect, drawing incredibly precise blueprints of the chest's structures. The lungs, being mostly air, can be tricky to image well, but CT cuts through this challenge brilliantly. It delivers razor-sharp, high-resolution pictures that map out the delicate, branching network of airways and blood vessels with stunning clarity.
CT: The Unrivalled Expert for Lung Tissue
When it comes to the lung tissue itself—what we call the lung parenchyma—CT is the undisputed champion. A massive part of its advantage is speed. A full chest scan can be done in a single breath-hold, which is crucial for minimising the blurring that breathing would otherwise cause.
This level of precision is absolutely vital for a few key jobs:
- Spotting Tiny Nodules: CT can pick up lung nodules just a few millimetres across, far smaller than anything a standard chest X-ray could ever hope to find.
- Characterising Lung Disease: For conditions like interstitial lung disease or emphysema, CT is fantastic at revealing the specific patterns of damage to the lung tissue.
- Diagnosing Emergencies: In an urgent scenario, like a suspected pulmonary embolism (a blood clot in the lungs), a specialised CT scan known as a CTPA (CT Pulmonary Angiogram) is the gold-standard diagnostic tool.
CT is our go-to for imaging the lung tissue itself. It gives us the architectural blueprint of the lungs, allowing us to spot even the smallest abnormality with confidence.
MRI: The Master of Soft Tissue Detail
Where CT excels in picturing the lungs' structure, MRI shines in an area where CT falls short: visualising soft tissues. MRI provides a level of detail and contrast between different soft tissues—muscle, fat, nerves, and tumours—that a CT scan simply can't replicate. It works by using a powerful magnetic field to get tissues to reveal their water content, creating images that are incredibly rich in information.
This unique ability makes MRI the better choice for looking at the structures around the lungs. It's invaluable for assessing mediastinal masses (tumours in the central part of the chest, between the lungs), evaluating chest wall tumours, and investigating certain complex cardiac issues, all without exposing the patient to any ionising radiation.
A Patient Story: Sarah’s Chest Wall Pain
Let me give you a real-world example. Sarah, a 42-year-old marathon runner, came to see me with a nagging pain on the right side of her chest wall. Her initial X-ray and even a follow-up CT scan didn't show anything definitive. The CT confirmed her lungs were clear and her ribs were fine, but it couldn't tell us what was causing the pain.
Based on the location and her symptoms, I had a hunch the problem was in the soft tissues of her chest wall, maybe a muscle or a nerve. So, we arranged an MRI. The scan revealed subtle inflammation and a small, benign tumour called a schwannoma growing from a nerve between her ribs—the clear source of her discomfort. The CT was essential to rule out lung problems, but it was the MRI that unlocked the correct diagnosis.
MRI gives us an unparalleled view of soft tissue, which is critical for surgical planning. When we need to know if a tumour is touching a vital nerve, blood vessel, or the heart, MRI provides the definitive answer.
This case really shows why the conversation isn't about which scan is "better." It's about choosing the right tool for the clinical question we're trying to answer. They are complementary, not competing, technologies, each offering a unique perspective.
Unfortunately, getting access to these essential scanners can be a real struggle in the UK, which lags well behind many of its European counterparts. As of 2021, the UK had just 10 CT scanners and 8.6 MRI units per million people—the lowest figures among 10 economically similar nations. This gap persists despite small increases in scanner numbers, highlighting the immense pressure on diagnostic services here. You can find out more from the British Medical Association data analysis.
Diagnosing Lung Cancer and Other Thoracic Conditions
When we're trying to diagnose a serious condition inside the chest, the choice between a CT scan and an MRI isn't arbitrary. It’s all about asking the right clinical question. Each scan gives us a unique window into the body, and knowing which one to use is how we build a clear, accurate picture, especially for something as critical as lung cancer.
For lung cancer, the diagnostic path is very well-trodden. A low-dose CT scan is, without question, the gold standard for both screening people at high risk and for the initial investigation of a suspicious lung nodule. Its incredible speed and the crystal-clear detail it provides of the lung tissue make it the definitive first-line tool.
This initial CT scan gives us the foundational information for any treatment plan.
- Tumour Size and Shape: We can precisely measure the dimensions of a nodule or mass.
- Exact Location: It pinpoints the tumour’s position within a specific lobe of the lung.
- Relationship to Airways and Vessels: Crucially, it shows if the tumour is getting close to major airways or blood vessels.
The Role of MRI in Lung Cancer Assessment
So, if CT is the workhorse, where does an MRI come in? While the CT tells us about the tumour itself, an MRI is often brought in to answer a very specific, and vital, follow-up question: has the cancer started to invade the surrounding soft tissues?
An MRI excels at showing the contrast and fine detail of non-bony structures. I'll typically order one to get a definitive view of:
- Chest Wall Invasion: Is a tumour growing into the muscles, fat, or nerves of the chest wall?
- Brachial Plexus Involvement: For tumours right at the top of the lung (what we call Pancoast tumours), an MRI can show if the cancer is affecting the delicate network of nerves running into the shoulder and arm.
- Spinal Cord Proximity: It can reveal if a tumour is pressing on or even invading the spine.
This level of detail is absolutely crucial for surgical planning. It helps us decide between minimally invasive surgery, a traditional open approach, or another course of treatment entirely. For patients, understanding why we're doing these specific tests can be reassuring. You can learn more about the importance of lung cancer screening in our detailed guide.
Patient Story: A Closer Look at Diagnosis
I recently saw a gentleman in his late 60s whose CT scan revealed a tumour right at the apex of his lung. The CT gave us a perfect map of the tumour inside the lung tissue, but its closeness to his spine was a major concern.
This is where the MRI was essential. It gave us exquisitely clear images showing a safe margin between the tumour and the critical nerve structures of his brachial plexus. This detail, which the CT simply couldn't provide, gave us the confidence to proceed with a minimally invasive keyhole procedure. For him, this meant a faster and much less painful recovery.
Diagnosing Other Common Thoracic Conditions
The distinct strengths of CT and MRI apply to a whole range of other chest conditions, not just cancer. The thinking is much the same—we match the scan’s capabilities to what we suspect is going on.
When we're investigating conditions of the lung tissue itself—things like pneumonia, infections, or fibrosis—a CT scan is the definitive tool. It provides the ground-truth images we need to make an accurate diagnosis and get treatment started.
For instance, when diagnosing a sudden, life-threatening event like a blood clot, CT is indispensable. When we discuss how CT scans visualise the chest, it's vital to recognise their role in identifying critical conditions such as a Pulmonary Embolus.
On the other hand, we often turn to MRI in situations where avoiding radiation or contrast agents is a priority, such as:
- Congenital Abnormalities: For younger patients with suspected chest wall or diaphragmatic issues they were born with.
- Vascular Issues: To evaluate certain blood vessel conditions without having to use iodinated contrast dye.
- Mediastinal Masses: To get a better look at tumours located in the soft-tissue-rich area between the lungs.
The demand for both types of imaging is soaring. NHS England data for 2022/23 shows that CT procedures hit 7.1 million (a 5.5% increase), while MRI scans reached 4.1 million (a 6.2% increase). These numbers really highlight the immense pressure on diagnostic services and why getting timely access is so important. You can explore more about these trends in the official NHS diagnostic imaging dataset.
Key Practical Differences: Radiation, Contrast, and Safety
When we're deciding between a CT and an MRI, the conversation quickly moves beyond just image quality. We have to consider the practical, real-world factors that directly affect you. The most common questions I get from patients revolve around radiation, the contrast dyes we use, and the overall safety of the procedure. These aren't just technical details; they are fundamental to choosing the right scan for your unique situation.
The big one, of course, is radiation. A CT scan uses ionising radiation—X-rays, essentially—to create its images. It’s important to keep this in perspective. Modern scanners are incredibly efficient and operate on the ALARA (As Low As Reasonably Achievable) principle. The dose from a chest CT is small and controlled, roughly equivalent to what you’d naturally absorb from the environment over a few years.
An MRI, on the other hand, uses no ionising radiation whatsoever. It works with powerful magnets and radio waves, making it an incredibly safe choice, particularly for younger patients or those who might need repeated scans over their lifetime.
Understanding Contrast Agents
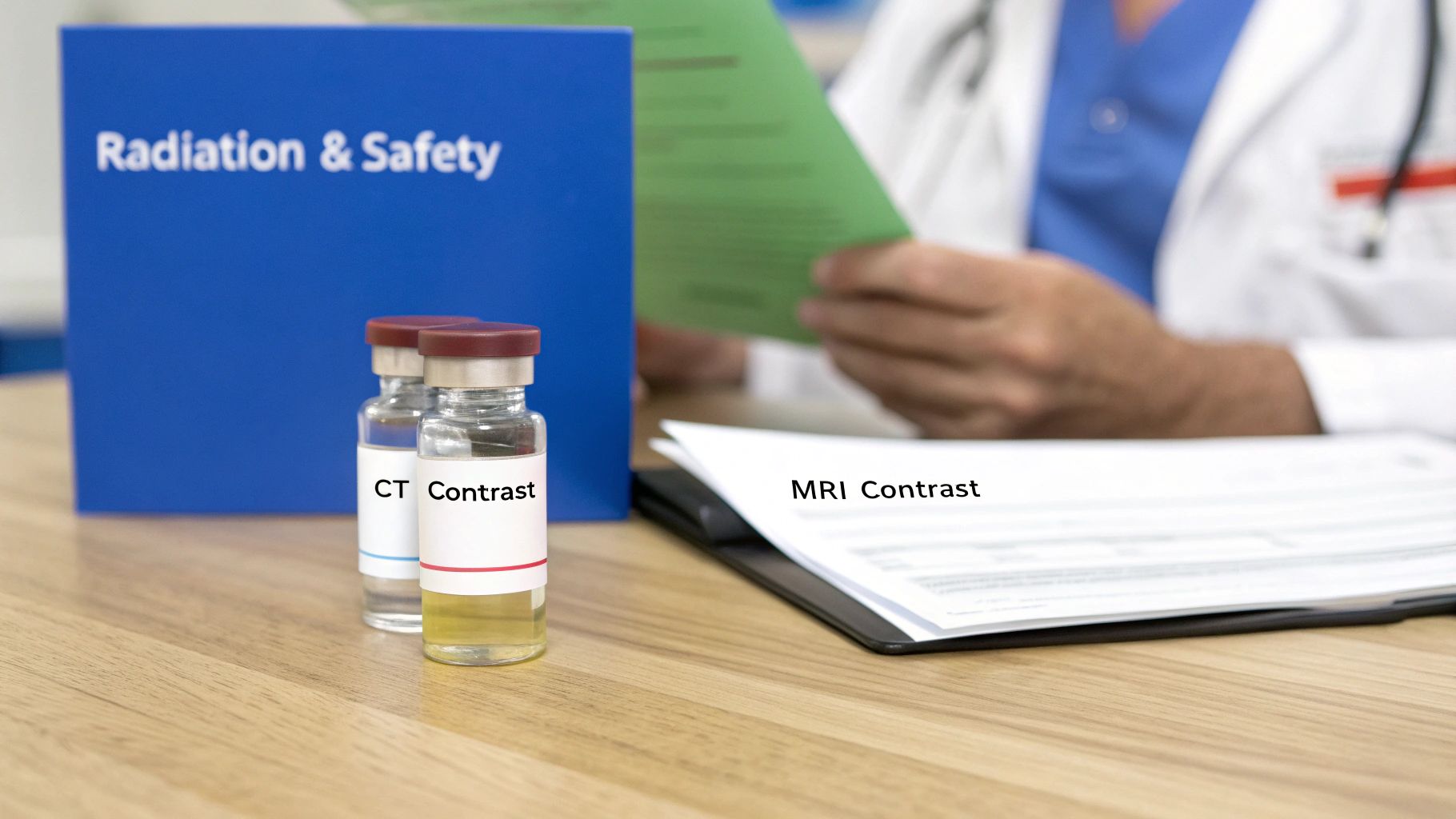
To get the sharpest possible images of certain structures, we often use a special dye known as a contrast agent. But the agents for CT and MRI are completely different, and that distinction matters.
- CT Scans rely on an iodine-based contrast. Injected into a vein, it can sometimes create a brief, warm flushing sensation or a metallic taste—both are normal and pass quickly.
- MRI Scans use a gadolinium-based contrast agent. This is also given intravenously but works in a different way to highlight tissues within the magnetic field.
Before any contrast is administered, your clinical team will run through some essential safety checks. We always check your kidney function with a simple blood test, because your kidneys are responsible for filtering the dye from your system. We'll also ask carefully about any allergies, as reactions, while rare, are always something we prepare for.
A Patient Story: Managing Contrast Safety
I recently had a patient, Mark, who needed a very detailed look at a tricky mass near his heart. His kidney function wasn't perfect, which made using the standard iodine contrast for a CT a potential risk. This is precisely the kind of scenario where the cat scan v mri decision pivots on patient-specific safety factors.
We opted for an MRI. This allowed us to use a gadolinium-based agent, which was much safer for his level of kidney function. The scan gave us the beautiful soft-tissue detail we needed to plan his operation meticulously, all without putting any extra strain on his kidneys. Mark’s case is a perfect example of how we tailor the imaging choice not just to the clinical question, but to the individual in front of us.
Patient safety is our absolute priority. We meticulously review kidney function and allergy history before any contrast-enhanced scan to ensure the benefits of a clearer diagnosis far outweigh any potential risks.
Absolute Contraindications: What You Need to Know
Finally, some pre-existing conditions or circumstances can make one type of scan unsuitable. We call these contraindications, and it’s why a full and honest medical history is so vital.
A quick overview of the safety considerations and practical differences is often helpful for patients and referrers.
Safety and Practical Factors: CT vs MRI
| Factor | CT (CAT Scan) | MRI |
|---|---|---|
| Radiation | Uses ionising radiation (X-rays). Dose is low and managed. | No ionising radiation. Uses magnets and radio waves. |
| Contrast Agent | Iodine-based. Potential risk with impaired kidney function. | Gadolinium-based. Different safety profile, often used when iodine is a concern. |
| Contraindications | Pregnancy (avoided unless essential), severe iodine allergy, significant renal impairment. | Metal implants (older pacemakers, clips), metal fragments in the body (especially eyes), claustrophobia. |
| Scan Time | Very fast—usually under 10 minutes for the entire process. | Longer—can take 30 to 60 minutes or more. |
| Noise & Comfort | Relatively quiet, open gantry (doughnut shape). | Can be very loud (requires ear protection), more enclosed space can trigger claustrophobia. |
This table summarises the key trade-offs. While a CT is incredibly fast, an MRI avoids radiation and may be safer from a contrast perspective for certain patients.
Knowing these practical differences empowers you to have a much clearer conversation with your specialist. It ensures the scan we choose is the perfect fit for your diagnostic needs and, just as importantly, for your personal health profile.
Navigating Your Scan in London and the NHS
Knowing the clinical pros and cons of CT and MRI is one thing, but getting your scan scheduled in a timely manner is a completely different challenge. For anyone in London, or indeed across the UK, the journey from a GP referral to getting your results means navigating the realities of the NHS. Understanding what to expect can make the whole process feel far less intimidating.
The NHS is making a commendable effort to boost its diagnostic capacity with Community Diagnostic Centres (CDCs). The idea is to bring scans closer to home, away from the hustle of major hospitals. While this initiative is growing, the reality is that most complex imaging, especially for thoracic conditions, still happens in a hospital.
The Current Reality of Getting a Scan
The numbers really paint a picture of the demand. In August 2024 alone, NHS England performed an incredible 723,243 CT scans and 398,199 MRI scans. But despite the national push to decentralise, only 8% of those CT scans and 13.5% of the MRIs actually happened in a CDC. That means just one in ten scans has so far moved to these newer community settings. You can read more about this in an in-depth health service analysis.
A Patient's Story: The Waiting Game
Think of someone like Maria, a 68-year-old from North London. An X-ray revealed a shadow on her lung, and her GP made an urgent referral for a CT scan. Even with the "urgent" tag, the wait was incredibly stressful. Every day without an appointment letter felt like a lifetime, fuelling a cycle of anxiety.
Maria’s experience is far from unique. The NHS staff work tirelessly, but waiting times are a huge source of worry for patients and their families. This period of limbo is often what prompts people to look at other options. For those who need answers more quickly, it’s worth understanding the different care pathways available. Our guide to NHS and private sector healthcare breaks this down in detail. Maria’s story is a powerful reminder of how important it is to be ready for the practical side of your diagnostic journey.
"The wait for my scan was the hardest part. Once I had the appointment, the actual procedure was quick and the staff were wonderful, but those weeks of not knowing were filled with anxiety. My advice is to have a list of questions ready for your doctor to feel more in control."
Preparing For Your Appointment
Whether your scan is at a large London teaching hospital or a local CDC, a little preparation can make all the difference to your experience.
- Confirm the Details: Always double-check the location, date, and time. Make a note of any specific instructions, particularly if you need to fast beforehand.
- Write Down Your Questions: Don't rely on memory. Jot down everything you want to ask about the scan, when you’ll get the results, and who will be explaining them to you.
- Bring a Companion: If you're feeling nervous, bringing a friend or family member for support can be incredibly reassuring.
Taking these small, practical steps can help you feel more empowered and less overwhelmed as you move forward with your diagnosis and treatment plan.
Your Questions Answered: Chest Scans Explained
Which scan is better for finding lung cancer: a CT or an MRI?
When it comes to detecting lung cancer, a low-dose CT (CAT) scan is unequivocally the gold standard. Its real strength lies in identifying tiny nodules within the lung tissue itself—often the very earliest sign of a problem.
An MRI has a different, more specific role. We typically use it after a cancer diagnosis has already been made. Its purpose is to determine if the tumour has invaded nearby soft tissues, such as the chest wall or the spine, which is crucial information for surgical planning. It's a supplementary tool, not the primary one for initial detection.
How long does a chest CT or MRI take?
This is a key practical difference. A CT scan of the chest is remarkably fast, with the scan itself usually completed in just 5-10 minutes.
An MRI, on the other hand, requires a bit more patience. The scan itself can take anywhere from 30 to 60 minutes. During this time, it's vital to remain as still as possible to ensure the images are sharp and clear.
Is the contrast dye used for CT and MRI scans safe?
Yes, for the vast majority of patients, both types of contrast agents are very safe. Before any scan involving contrast, our team will always review your medical history, specifically checking your kidney function and asking about any known allergies to mitigate any potential risks.
It's worth knowing they are different substances. CT scans use an iodine-based contrast, while MRIs use a gadolinium-based one. It’s common to feel a temporary, warm sensation as the dye is administered, but serious allergic reactions are extremely rare. Rest assured, the clinical team is always fully prepared to manage any adverse effects immediately.
If you're facing a diagnosis and need answers quickly, Marco Scarci Thoracic Surgery offers rapid access to consultations and minimally invasive surgical options. Learn more about how we can help you by visiting marcoscarci.co.uk.