Discovering a new lump or swelling on your chest can be alarming. It’s a natural reaction. This growth, known as a chest wall lump, can appear on any of the structures that form the protective cage around your heart and lungs—the ribs, sternum (breastbone), cartilage, and muscles. While it's easy to assume the worst, it's important to remember that many of these lumps are benign (non-cancerous).
Even so, you should always have any new lump checked by a doctor. Getting a professional medical opinion is the only way to find out what’s causing it and get the peace of mind you need.
Understanding a Lump on Your Chest Wall

Finding an unexpected lump on your chest is an unsettling experience that immediately triggers a wave of questions and anxiety. Let's start with the basics: what exactly is the chest wall? Think of it as the protective armour for your vital organs, primarily your heart and lungs. It’s a sophisticated structure built from bone (your ribs and sternum), flexible cartilage, and several layers of muscle.
Because a lump can originate from any of these different tissues, its feel and characteristics can vary dramatically from one person to another. This guide is here to cut through the confusion, offering clear, reassuring information about what to expect and the steps you need to take.
A Patient's Story: From Worry to Reassurance
To put this all into perspective, let's follow the story of a patient I recently treated. He was a fit and healthy man in his 40s who discovered a firm, golf-ball-sized lump on his chest while getting dressed. His mind, like many people's would, immediately jumped to the worst possible conclusion.
His journey—from that first jolt of fear to receiving a clear, manageable diagnosis—offers a real-world look at this process. His story underscores a critical point: the anxiety of not knowing is often the hardest part. You can hear his full story in his own words in the video below. For another personal account, reading about Anita's journey of discovering a breast lump provides valuable insight into the emotional and practical first steps.
The single most important thing you can do after finding a chest wall lump is to seek a professional medical opinion. Early assessment is the key to an accurate diagnosis, effective treatment, and, crucially, your own peace of mind.
Waiting and worrying achieves nothing. Taking control by booking an appointment with your GP is the most powerful first step you can take. It’s about turning that feeling of uncertainty into a clear, proactive plan.
This guide will walk you through everything you need to know, from common causes and diagnostic tests to the latest treatment options. While a lump can sometimes be linked to structural issues, like those we cover in our overview of common chest wall deformities, only a proper evaluation can tell you for sure. Understanding the process will help you face it with confidence.
Common Reasons for a Benign Chest Wall Lump
The moment you find a lump on your chest wall, your mind can easily jump to the worst-case scenario. It’s a completely natural reaction. But here’s some immediate reassurance: the vast majority of these lumps are benign. That means they’re not cancerous and don’t pose a serious threat to your health.
Think of it this way—your body is a complex structure, and sometimes harmless growths just appear. They can spring from different tissues like fat, skin, or connective fibres, which is why they can all feel so different. Getting to know the common culprits can go a long way in easing that initial wave of anxiety.
Lipomas: Soft and Mobile Lumps
One of the most frequent things we see is a lipoma. In simple terms, this is just a slow-growing collection of fat cells that forms a soft, rubbery lump just under the skin. Most people describe them as feeling a bit ‘doughy’, and they’re usually painless.
The tell-tale sign of a lipoma is that it’s mobile. If you gently push on it, you’ll likely feel it shift around quite easily beneath your skin. While they can pop up almost anywhere, the chest wall is a common spot. For most people, they are more of a cosmetic nuisance than a medical problem and often don't need any treatment at all unless they start to hurt or get noticeably larger.
Fibromas and Cysts: Firm but Harmless
Another common type of benign growth is a fibroma, which is made up of fibrous or connective tissue. Unlike the softness of a lipoma, a fibroma tends to feel quite firm, sometimes even hard. They are typically small, grow very slowly, and rarely cause any pain.
Cysts are also a regular find. A cyst is essentially a small, closed sac that can be filled with fluid, air, or other material. Epidermoid cysts, for example, come from skin cells and are filled with a thick substance called keratin. They’re usually harmless, but can become a bit tender or inflamed if they get irritated or infected.
The reassuring reality is that benign chest wall lumps vastly outnumber malignant ones. While every lump needs a proper evaluation, statistics show that panic is often unnecessary.
Data from clinical practice here in the UK really backs this up. Primary chest wall tumours are rare, and of those that do occur, around half are benign. This is exactly why getting checked is so important—it’s the step that separates a harmless bump from something more serious, but the odds are very much in your favour. For those interested in the numbers, you can explore the research behind chest wall tumour statistics to get a deeper understanding.
To help you get a clearer picture, here’s a quick comparison of the most common benign lumps you might encounter.
Comparing Common Benign Chest Wall Lumps
| Lump Type | Typical Feel | Mobility | Common Symptoms |
|---|---|---|---|
| Lipoma | Soft, rubbery, or ‘doughy’ | Moves easily under the skin | Usually painless; can be a cosmetic concern |
| Fibroma | Firm, solid, or hard | Generally fixed in place | Typically no pain; slow-growing |
| Cyst | Smooth, firm lump; may feel like a small pea | Can be mobile or fixed | Can become red, tender, or inflamed if infected |
Remember, this table is just a guide. The only way to be certain about the nature of a lump is through a proper medical evaluation.
A Patient's Story: Sarah's Lipoma
Let me tell you about Sarah, a 42-year-old teacher who found a soft, movable lump on her rib cage while she was at the gym. Her GP thought it was likely a lipoma, but to be absolutely sure, he referred her for an ultrasound—standard practice.
The scan confirmed it: a classic, harmless fatty lipoma. The relief Sarah felt was immense. A few months later, she decided to have it removed with a simple minor procedure, but only because it was in a spot where her bra strap was constantly rubbing it. The choice was entirely hers. Sarah’s story is a perfect example of how a worrying discovery often ends with a straightforward and reassuring outcome.
Understanding these common causes can provide some much-needed context, but it's no substitute for a professional diagnosis. True peace of mind only comes when a specialist has properly examined your chest wall lump and can tell you exactly what it is.
When a Chest Wall Lump Needs Urgent Attention
While most lumps are nothing to worry about, it’s crucial to know the signs that suggest something more serious might be going on. Think of a change in a lump's size, feel, or appearance as your body's way of telling you it's time to get it checked out. Ignoring these signals can lead to delays in diagnosis and treatment, which is why understanding the red flags is so important.
Sometimes, a chest wall lump is a sign of a cancerous growth. These fall into two main camps. The first are primary chest wall tumours—cancers that start directly in the bone, cartilage, or soft tissues of the chest wall itself. These are pretty uncommon but absolutely require specialist attention.
The second type are secondary tumours, often called metastases. This is when cancer cells from a tumour somewhere else in the body, like the lung, breast, or kidney, break away. They then travel through the bloodstream or lymphatic system and set up a new tumour in the chest wall.
The Red Flag Symptoms to Watch For
When your GP examines a lump on your chest wall, they are looking for specific characteristics. These are often called ‘red flag’ symptoms because they signal that the lump needs a much closer, more urgent look. If you notice any of the following, it’s best to make an appointment with your doctor right away.
Key warning signs include:
- Rapid Growth: A lump that gets bigger over a few weeks or months is a major red flag. Benign lumps like lipomas tend to grow incredibly slowly, if they grow at all.
- Hard and Fixed Texture: If the lump feels hard, dense, and seems stuck to the tissue or bone underneath—rather than moving around freely under the skin—it needs investigating.
- Skin Changes: Keep an eye out for any changes to the skin over the lump. This could be redness, dimpling (a bit like an orange peel), warmth to the touch, or an open sore (ulceration) developing.
- Associated Symptoms: A lump that comes with other unexplained symptoms—like persistent pain, losing weight without trying, fevers, or night sweats—should always be checked out promptly.
These signs don't automatically mean it's cancer, but they are serious enough to warrant an urgent referral for more tests. Time and again, we see that catching things early leads to better outcomes, so your awareness and quick action really do make all the difference.
A Patient's Story: David’s Urgent Referral
Let's go back to David, a 55-year-old who found a firm lump near his ribs. At first, he hoped it was just a harmless cyst. But over the next month, he couldn't ignore that it seemed to be getting slightly bigger and felt completely solid, almost like a little stone under his skin.
When his GP examined him, two things stood out: the lump was hard, and it didn't move when she pressed on it. It felt anchored to the rib below. These features, along with its recent growth, were enough to trigger an urgent two-week referral for an ultrasound scan. David’s story is a perfect example of how spotting these red flags is the first, vital step on the diagnostic path.
As a guiding principle in clinical practice, a chest wall mass in anyone over the age of 40 should be considered malignant until proven otherwise. This underscores the importance of a swift and definitive diagnosis through imaging and, if necessary, a biopsy.
Understanding Chest Wall Sarcomas
Primary chest wall tumours, especially soft tissue sarcomas, are rare but can be aggressive. Because they are so uncommon, getting a diagnosis from a specialist team is essential. As we explain in our guide to thoracic sarcomas, these tumours grow from the body’s connective tissues.
The statistics really highlight why we need to be so vigilant. In England, Cancer Research UK reports around 4,600 new cases of soft tissue sarcomas each year. For adults, chondrosarcomas (which start in cartilage) are a common type found in the chest wall, while Ewing's sarcoma is seen more often in children and young adults.
Due to how serious these can be, NICE guidelines ensure anyone with a suspicious lump is fast-tracked for diagnostic imaging—usually an ultrasound or CT scan—within two weeks. You can read more about the UK statistics on soft tissue sarcomas to get a fuller picture.
Knowing the red flags for a chest wall lump isn’t about causing alarm. It’s about giving you the knowledge to act decisively for your own health.
Your Diagnostic Journey: From First Visit to a Clear Answer
Finding a lump on your chest wall can feel like discovering a puzzle you never wanted to solve. It’s a journey that naturally comes with questions, tests, and anxious waits. My goal here is to walk you through that entire process, step by step, so you know exactly what’s happening and why. We’ll turn the unknown into a clear, manageable path.
Let's follow the story of David, whom we met earlier. His GP spotted a few red flags—a hard, fixed lump that was getting bigger—and immediately put him on an urgent two-week referral pathway. This is standard practice in the UK for any suspicion of something serious, ensuring you’re seen by a specialist as quickly as possible.
The First Step: Your GP Consultation
It all starts with your GP. This first appointment is crucial because it sets the direction for everything that follows. Your doctor will want to hear the full story: when you first noticed the lump, if it’s changed in size or texture, and whether you have any other symptoms, like pain or unexplained weight loss.
Next comes the physical examination. Your GP will gently but thoroughly feel the lump to get a sense of its characteristics:
- Size and Shape: Is it small and round, or larger and more irregular?
- Texture: Does it feel soft and squishy like a lipoma, or is it firm and unyielding?
- Mobility: Can it be moved around easily under the skin, or does it feel stuck to the tissue or bone beneath?
- Skin Changes: Is there any redness, swelling, or unusual dimpling of the skin over the lump?
Based on what they find, your doctor will decide what to do next. For David, the hard, fixed nature of his lump was enough to justify an immediate referral for imaging. This kind of decisive action is vital for getting to the bottom of things without delay.
Imaging Tests: Peering Inside the Lump
Think of imaging tests as a specialist's high-tech torch, letting them see what's going on under your skin without making a single cut. The type of scan you'll have depends on the clues your lump has already provided.
The first port of call is usually an ultrasound scan. It’s a simple, completely painless procedure that uses sound waves to create a live picture of the lump and its surroundings. Ultrasound is fantastic at telling us whether a lump is solid or filled with fluid (a cyst). For many benign lumps, an ultrasound might be all that’s needed to provide a confident diagnosis.
However, if the ultrasound reveals a solid mass or there are other features that need a closer look, your doctor will likely arrange for more detailed scans.
- CT (Computed Tomography) Scan: A CT scan uses X-rays to create detailed, cross-sectional images of your chest. It’s especially good at showing how the lump relates to your bones—like the ribs and sternum—and can also check for any spread to nearby lymph nodes or organs.
- MRI (Magnetic Resonance Imaging) Scan: An MRI uses powerful magnets and radio waves to generate incredibly detailed pictures of soft tissues. It's the best tool for characterising the precise nature of a lump, giving us a crystal-clear view of muscles, fat, and other connective tissues.
During your diagnostic journey, you might undergo various imaging tests; it's helpful to know what to expect, for instance, when facing the prospect of understanding a callback mammogram, a situation many people encounter.
The image below shows some of the key red flags that often lead to these more advanced imaging tests.
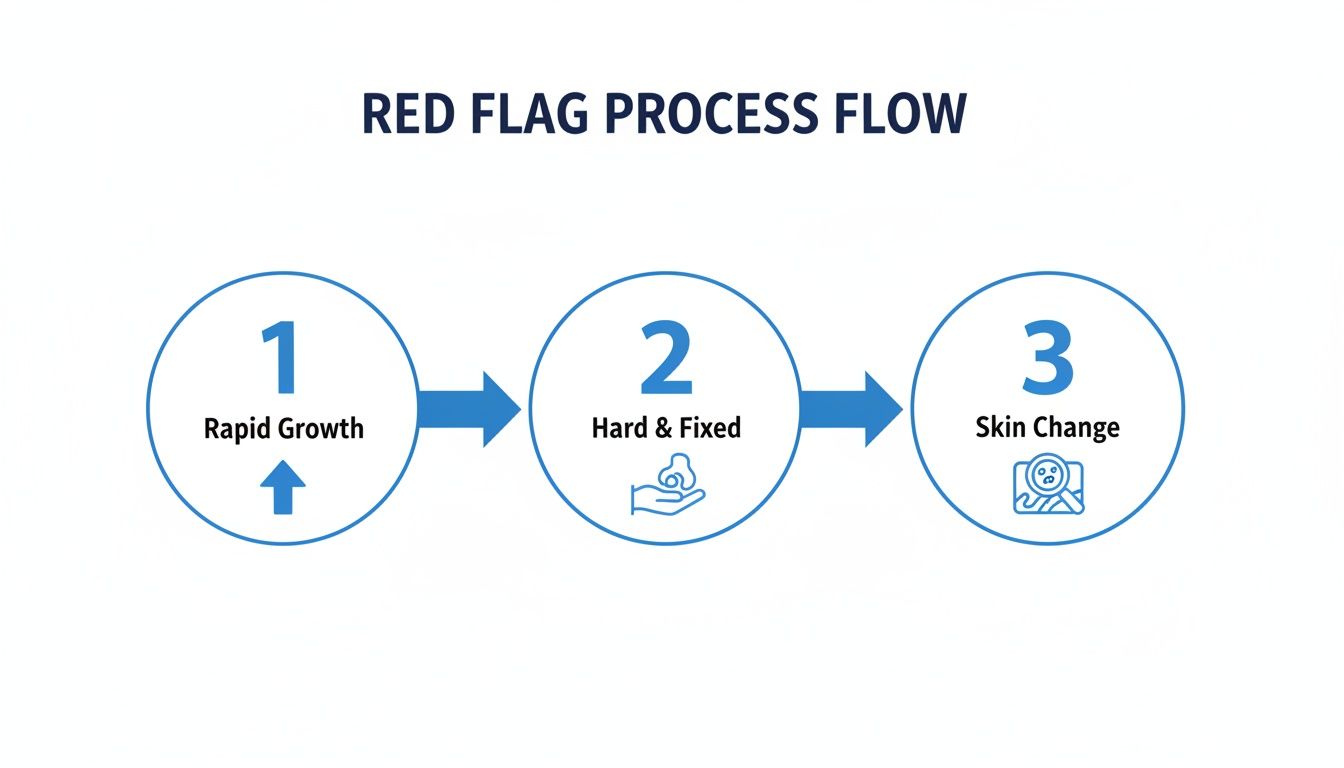
This flow chart highlights why symptoms like rapid growth or a hard texture are such critical signposts that guide us down the right diagnostic path.
The Biopsy: Getting the Definitive Answer
While scans give us a huge amount of information about a lump’s size, location, and structure, they can’t always tell us the full story. To know for certain what a lump is made of, we often need a biopsy. This is the gold standard for diagnosis. It involves taking a very small tissue sample directly from the growth, which is then sent to a pathologist to be examined under a microscope.
A biopsy is the only way to definitively confirm or rule out cancer. It allows doctors to identify the exact type of cells within the lump, which is essential for creating an effective treatment plan.
There are a few ways to perform a biopsy, but a core needle biopsy is very common. It’s usually done under local anaesthetic. A doctor uses an ultrasound or CT scan to guide a special hollow needle right into the lump to remove a tiny core of tissue. The procedure is quick, and that small sample provides the final, crucial piece of the diagnostic puzzle.
If you are experiencing other related symptoms, you might find it useful to read our guide on the 7 key insights on chest and rib pain. Knowing what to expect at each stage, from the initial exam to the final biopsy result, can help you feel more in control and reduce the stress of the unknown.
Modern Treatment Options for Chest Wall Lumps

Once we have a definitive diagnosis for your chest wall lump, the uncertainty fades and we can map out a clear plan. The right path forward depends entirely on what the tests have shown us – the lump's type, its size and location, and, most importantly, whether it's benign or cancerous.
For many harmless growths, like a small lipoma that isn't causing any trouble, the best approach is often just to keep an eye on it. This "watchful waiting" means we monitor the lump over time, avoiding an operation you don't need. If, however, a benign lump starts to cause pain, gets bigger, or you simply don't like the look of it, a straightforward surgical removal is a very effective option.
But when a chest wall lump turns out to be malignant, a more structured, team-based approach is absolutely essential. This is where the Multidisciplinary Team (MDT) becomes the cornerstone of your care.
The Power of Collaborative Care
In the UK, it’s the gold standard for any cancer diagnosis to be discussed at an MDT meeting. This isn't just one doctor making a call; it’s a dedicated group of specialists. Thoracic surgeons, oncologists, radiologists, and pathologists all sit down together to review every detail of your case, combining their expertise to build a treatment plan that’s right for you.
This collaborative process makes sure every angle is covered, from the best surgical strategy to whether you might also need chemotherapy or radiotherapy. It ensures your care is coordinated, seamless, and built around your specific situation.
A Patient’s Story: David’s Personalised Plan
Let’s go back to David’s story. His biopsy confirmed a primary chest wall sarcoma, a cancer that begins in the soft tissue. The MDT carefully reviewed his scans and pathology reports, concluding that the tumour was contained and hadn't spread. This made surgery the most effective first-line treatment.
The team recommended a complete surgical excision. The goal here is to remove the tumour along with a safe margin of healthy tissue around it to ensure no cancer cells are left behind. For David, this involved taking out the tumour, a small piece of the affected rib, and some surrounding muscle, followed by a chest wall reconstruction to restore stability.
The goal of modern thoracic surgery is not just to remove the problem, but to do so in a way that minimises the impact on the patient's body, reduces pain, and speeds up their return to normal life.
This guiding principle is what helps us choose between traditional open surgery and newer, minimally invasive techniques. While open surgery still has its place, we now lean towards these advanced methods because of the significant benefits for patients.
Advanced Surgical Techniques
When an operation is needed for a chest wall lump, we have sophisticated options that are a world away from the large incisions of the past.
- Video-Assisted Thoracic Surgery (VATS): This is a keyhole technique where we make a few small incisions. A tiny camera (a thoracoscope) and specialised instruments are passed through these ports, allowing me to perform the operation with immense precision while watching on a high-definition screen.
- Robotic Surgery: This takes keyhole surgery to the next level. I sit at a console and control highly precise robotic arms to perform the procedure. The system gives me an enhanced 3D view and a level of dexterity that surpasses the human hand, making it possible to carry out incredibly complex operations through tiny incisions.
Both VATS and robotic surgery offer huge advantages over traditional open surgery, including less pain, smaller scars, a shorter hospital stay, and a much faster recovery.
A robotic-assisted approach was the best choice for David. It allowed for the precise removal of his tumour and the rib section while minimising trauma to the surrounding healthy tissue. As a result, his recovery was far quicker and less painful than it would have been with a large open operation.
In the UK, lung cancer can sometimes grow into the chest wall, creating lumps that might be mistaken for something less serious. That's why NICE guidelines recommend a two-week ultrasound for any unexplained lump in an adult – it helps catch these malignancies early. Alarms bells like a growing lump or a history of smoking will trigger an urgent cancer pathway referral. Without quick action, these tumours can invade deeper, making surgery far more complex. You can find out more about the importance of early investigation for chest wall masses.
Your Pathway to Private Thoracic Care
Discovering a lump on your chest is naturally worrying, and the waiting that often follows can be the hardest part of all. If you're looking for faster answers and a direct route to a specialist, the private healthcare system offers a clear path. It's about getting the reassurance you need, when you need it, without the stress of long delays.
The single biggest advantage of going private is speed. You can bypass the lengthy referral queues and get straight to a senior thoracic surgeon. This means your consultation, any necessary scans, and potential treatment can all happen in a much shorter, more manageable timeframe, significantly cutting down that period of uncertainty.
A Patient's Story: Sarah's Journey to Peace of Mind
Take Sarah, a 48-year-old marketing executive who found a firm, painless lump on her chest. Her GP was reassuring, but the prospect of a long wait for scans left her feeling incredibly anxious. On a colleague's recommendation, she decided to book a private consultation directly.
Within a few days, Sarah was in my office discussing her concerns. We arranged an MRI scan for her later that same week, which confirmed the lump was a benign fibroma – completely harmless. The entire process, from her initial discovery to a definitive diagnosis, took just over a week. That swift, coordinated care gave her enormous peace of mind and let her get back to her life without the shadow of worry.
"When you find a lump, all you want are answers. The ability to see an expert quickly, have all the tests coordinated, and get a clear diagnosis without delay is invaluable. It transforms a period of high anxiety into a manageable process."
Using Private Medical Insurance and Self-Funding Options
Many of my patients use private medical insurance to cover their consultations and treatment for conditions like a chest wall lump. It's usually a very straightforward process:
- Speak to your GP: Most insurance companies will ask for a referral letter from your GP before they authorise specialist care.
- Get an Authorisation Code: Once you have the referral, call your insurer. They will give you a pre-authorisation code for the consultation and any follow-up tests.
- Book your Appointment: With that code, you can book your appointment directly with my practice.
If you don't have insurance, self-funding is a direct and transparent alternative. My team provides a clear, itemised quote for consultations and any procedures you might need, so there are no hidden surprises. We can also discuss financing options to make private care more accessible. Ultimately, our goal is to ensure that anyone seeking prompt, expert care can get it when it matters most.
Your Questions Answered: Making Sense of a Chest Wall Lump
Finding a lump on your chest naturally brings up a lot of questions. It's completely normal to feel a bit anxious. Here, I'll tackle the most common concerns I hear from patients, giving you straightforward answers to help clear up the uncertainty.
Is it normal for a chest wall lump to hurt?
Yes, pain is certainly possible, but it’s a surprisingly unreliable clue. A simple, inflamed cyst or even a minor knock to a rib can be incredibly tender, while something more serious might not hurt at all.
Many cancerous growths, for instance, are completely painless when they first appear. That’s why the most important thing to remember is this: any new lump, painful or not, needs to be checked by a doctor. Don't let the absence of pain give you a false sense of security.
How soon should I get a lump checked?
My advice is always to book an appointment with your GP as soon as you find a new lump or notice a change in an existing one. Most turn out to be nothing to worry about, but getting it checked is the only way to be sure and get that peace of mind.
You should push for an urgent appointment if you spot any 'red flag' signs. This includes things like the lump growing quickly, feeling very hard and stuck in one place, or if the skin over it looks different. These symptoms need investigating right away.
A Patient's Story: Mark's Reassurance
Mark, a 62-year-old, found a small, hard lump on his sternum. Worried about a long wait, he opted for a private consultation. We arranged an MRI for him within two days, and the results quickly confirmed it was a benign cartilage growth. Mark's experience shows how getting fast answers can prevent weeks of unnecessary stress.
What's the difference between a CT and an MRI scan?
Think of them as two different tools for looking inside the body, each with its own speciality. A CT scan is brilliant for looking at bone. It uses X-rays to create a detailed picture, so it's the go-to scan if we need to see if a lump is affecting your ribs or sternum.
An MRI, however, uses magnets and gives us an incredibly clear view of soft tissues – things like muscle, fat, and the specific texture of the lump itself. It’s not uncommon to use both. By combining the information, we can build a really precise, three-dimensional understanding of what’s going on, which is key to an accurate diagnosis.
If a chest wall lump is causing you concern and you'd prefer not to wait, the team at Marco Scarci Thoracic Surgery is ready to help. We provide fast-track consultations and diagnostics to give you clear answers and a personalised plan without the usual delays. Learn more about booking your consultation.