You’re not imagining it. That sharp, stabbing pain under your rib cage—the one doctors keep misdiagnosing—has a name. It’s called Slipping Rib Syndrome (SRS), and if you’re reading this, there’s a good chance you’ve been chasing answers for far too long.
Let’s break it down in plain, human terms—what it is, how to know if you have it, and what you can actually do about it.
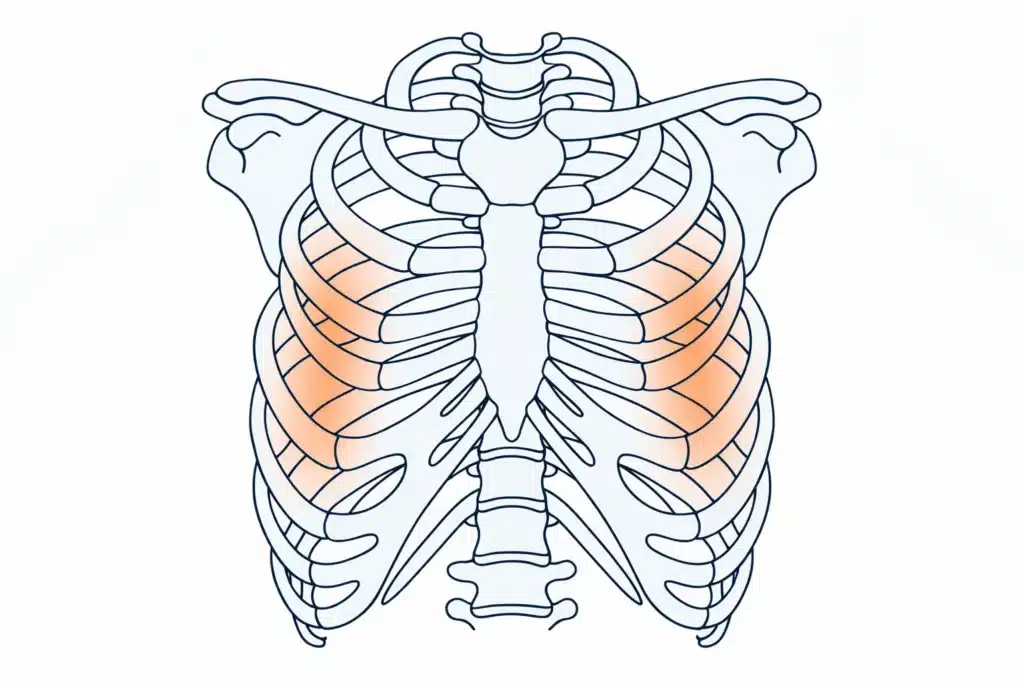
This condition is also called Cyriax syndrome, twelfth rib syndrome, rib tip syndrome, rib subluxation, or painful rib syndrome. Your ribcage isn’t as rigid as you might think. Your upper ribs anchor firmly to your breastbone, while your lower chest ribs—the 8th, 9th, and 10th—connect through softer tissue. These are your “false ribs.” In some people, especially after an injury or years of repetitive motion, the ligaments that hold these ribs can become loose. That’s when the rib starts to shift—”slipping”—and irritates nearby nerves and muscles because of excessive movement.
That slipped rib creates sudden, sharp pain. Sometimes it clicks. Sometimes it feels like something is stuck or stabbing you with severe pain afterward. And for most, it’s hard to describe without sounding dramatic. That’s one of the reasons this condition often gets misdiagnosed or overlooked. Pain that moves, doesn’t show up on standard imaging, and doesn’t match textbook definitions? That’s why many doctors don’t consider slipping rib syndrome as a possibility, since they lack the training to diagnose it.
This abnormal movement irritates the intercostal nerves, muscles, and connective tissue, leading to inflammation and discomfort. Such rib displacement distinguishes Slipping Rib Syndrome from other causes of chest wall pain.
Most doctors don’t spot it right away. Why? Because the symptoms mimic a dozen other conditions—heartburn, pulled muscles, even heart issues. And unless your provider knows what to look for, SRS might not even be on their radar.
Here’s the typical journey many patients take:
the ER visit for chest pain, followed by blood tests, X-rays, EKGs—all normal. Next stop: cardiologist, gastroenterologist, perhaps even a pain clinic. Each one rules out something serious, but no one can quite pinpoint the cause. And then the emotional toll kicks in. You start doubting yourself.
Is it anxiety? Am I making this up?
Many patients bounce between specialists before someone finally says the words:
“I think you have Slipping Rib Syndrome.”
That moment, for many, feels like relief and validation all at once.
The average time to a correct diagnosis can be years, not weeks. Patients often feel dismissed, told their pain is psychosomatic or stress-related, simply because the usual tests don’t show anything. In reality, experienced chest wall syndrome providers spot it.
Anyone can develop SRS, but certain groups are more prone:
Athletes in high-twist sports: swimmers, golfers, tennis players, rowers
Dancers and gymnasts, whose training often emphasizes hypermobility
Manual laborers, especially those who lift, twist, or reach overhead frequently
People with hypermobility or connective tissue disorders, like Ehlers-Danlos Syndrome
Postpartum individuals: due to changes in connective tissue and body mechanics
Anyone who’s had recent trauma, including car accidents, falls, or even aggressive coughing
Interestingly, some people develop symptoms without an apparent injury. Genetics, lifestyle, and even posture can all contribute to weakened ligaments around the rib joints.
Anyone can develop SRS, but certain groups are more prone:
Athletes in high-twist sports: swimmers, golfers, tennis players, rowers
Dancers and gymnasts, whose training often emphasizes hypermobility
Manual laborers, especially those who lift, twist, or reach overhead frequently
People with hypermobility or connective tissue disorders, like Ehlers-Danlos Syndrome
Postpartum individuals: due to changes in connective tissue and body mechanics
Anyone who’s had recent trauma, including car accidents, falls, or even aggressive coughing
Interestingly, some people develop symptoms without an apparent injury. Genetics, lifestyle, and even posture can all contribute to weakened ligaments around the rib joints.
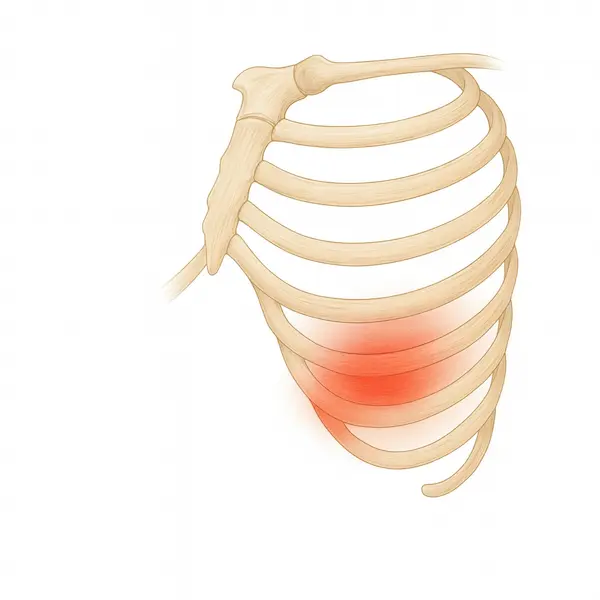
Sharp, stabbing pain under your lower ribs
A popping or clicking feeling or slipping sensation when you twist, bend, or breathe deeply
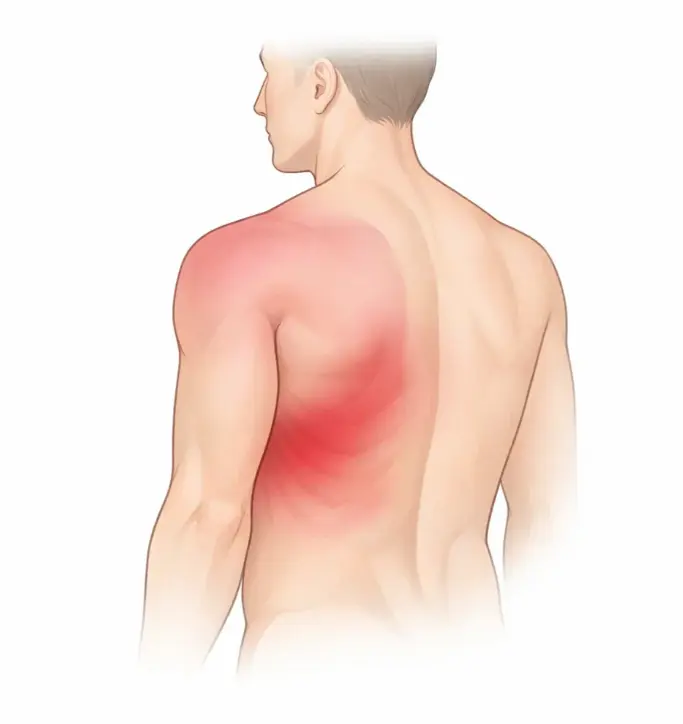
Pain that radiates to your back, side, or upper abdomen
A sense of pressure or instability in your ribcage
Worsening pain with certain positions—like lying on one side or getting out of bed
Fear of movement due to unpredictable pain
Difficulty breathing
Upper abdominal pain is mistaken for digestive issues
Shoulder or arm pain resembling nerve entrapment
Anxiety or panic due to breath-restricted pain episodes
Referred pain to the chest or flank, mimicking gallbladder or cardiac issues
Ask your provider about the Hooking Maneuver—a test where they hook their fingers under your rib edge and gently pull. If that triggers your pain or a click, it’s a big red flag for SRS.
Also helpful: Dynamic ultrasound (not just X-rays), which shows ribs in motion. This imaging, when paired with a skilled physical exam, is often more helpful than MRIs or CT scans.
You may also encounter these diagnostic tools:
Physical Therapy (PT): A targeted program should strengthen the muscles that support your ribcage and spine. Therapists may focus on breathing mechanics, posture retraining, core stability, and neuromuscular control. Manual therapy may also include soft tissue work or taping techniques to support the area.
Pain management: This may include ice during flare-ups, heat to ease muscle tension, and over-the-counter medications like ibuprofen. Topical options—like lidocaine patches or anti-inflammatory creams—can also help calm the area.
Movement modifications: Learn your triggers. If twisting to reach overhead causes pain, swap how you move. Modify workouts, adjust workstations, and avoid positions that stretch or torque your ribs until you’re stronger.
Postural re-education: Many patients unknowingly slouch or compensate to avoid pain, which creates further imbalances.
When pain persists despite conservative care, your medical team may explore these options:
Corticosteroid injections: These reduce inflammation around the slipping rib. Some patients get relief for several months.
Intercostal nerve block: These target the nerves running between your ribs. Relief is temporary, but can confirm SRS as the pain source.
Prolotherapy: A regenerative injection technique that helps stimulate tissue repair and ligament strengthening
Pain management specialists, orthopedic physicians, or sports medicine doctors familiar with musculoskeletal nerve pain often perform these interventions.
Surgeons may recommend surgery if your quality of life suffers and nothing else helps:
Costal cartilage resection: Removing part of the floating rib that allows it to slip
Rib stabilization: Using sutures, mesh, or titanium clips to hold the rib in place, eliminating any rib instability
Some surgeons also remove intercostal nerves during the procedure if chronic nerve pain is present. Surgical outcomes vary, but when done by experienced thoracic surgeons, many patients report dramatic improvement in pain and function.
Recovery from surgery usually includes several weeks of rest followed by physical therapy to restore normal motion and strength.
This condition isn’t just physical—it wears on you emotionally. Patients report feeling dismissed, frustrated, and even gaslit by years of being told “it’s just stress” or “there’s nothing wrong.”
"It felt like someone had a knife between my ribs every time I moved. I saw five specialists before one finally gave it a name. By then, I had stopped doing yoga, driving long distances, and even sleeping on my side. I felt like a different person."
“I used to avoid hugs, laughing, and sneezing. That’s how unpredictable the pain was. I lived in fear of motion. Once I got a diagnosis and started PT, my life changed.”
If this sounds like your story, you’re not alone—and you’re not crazy. One of the most healing things for patients is simply learning there’s a name for what they’ve been feeling. A real diagnosis. A path forward.

It’s not a weakness to avoid specific movements—it’s innovative management.

Use pillows to prop your side, keep your ribs supported, and avoid deep torso twists.

Inflammation can worsen symptoms. A diet low in processed foods and rich in anti-inflammatory nutrients may help overall healing.

Movement improves circulation and strength, but avoids high-impact or rotational activities until cleared.

Noting what causes or eases your pain can help your provider fine-tune treatment.

Some patients find relief with gentle rib braces or wraps that offer support during activity.

Chronic pain can trigger anxiety, depression, or isolation. Therapy or support groups help more than you think.
Getting properly diagnosed and treated can feel overwhelming, especially if insurance doesn’t fully cover every step. Here’s what you might expect:
£75–£200 per session without insurance (10–20 sessions recommended)
£300–£1,000
£500–£1,500 depending on the number and location
£5,000–£15,000+, depending on surgeon, hospital fees, and whether it’s outpatient.
Check if local teaching hospitals offer reduced fees for diagnostics
SRS can flare during hormonal changes (e.g., menstrual cycles, menopause)
It’s possible to have multiple ribs affected, not just one
Some people with SRS also report issues like costochondritis (inflammation of rib cartilage)
Many online support groups offer helpful tips and emotional support—search "slipping rib syndrome support" on Facebook or Reddit
Chiropractic and osteopathic adjustments can sometimes worsen symptoms—proceed with caution
Massage therapy, acupuncture, and dry needling sometimes relieve symptoms, but results vary
Staying informed helps: Reading peer-reviewed articles and patient stories online can empower you to have better conversations with your provider
If you’ve been living with undiagnosed rib pain, don’t give up. Print this out. Please bring it to your doctor. Ask about the Hooking Maneuver. Insist on being taken seriously.
The road to recovery might take time, but once you have the right name for what’s going on, you can finally start healing.
You remain intact. You only need the proper diagnosis.
Contact me today to schedule your consultation. Your journey to better health starts with a single phone call.
Take the first step towards expert thoracic care. Dr. Scarci's minimally invasive surgical techniques offer the best chance for successful outcomes with faster recovery times.
London, UK
Multiple clinic locations available
24/7 emergency support available