Introduction to craniofacial hyperhidrosis
Craniofacial hyperhidrosis is characterized by excessive, uncontrollable sweating of the face, head, and/or scalp, independent of temperature or physical activity. This page is intended for individuals experiencing excessive facial or scalp sweating and those seeking NHS treatment options. Craniofacial hyperhidrosis is a type of excessive sweating that affects the face and scalp. Excessive sweating can develop at any age but often starts in childhood or puberty. The most common type of hyperhidrosis affects certain body sites only, including the face and scalp.
Craniofacial hyperhidrosis NHS refers to the specific recognition, diagnosis, and management of this condition within the NHS, ensuring that patients receive appropriate care and support. Unlike generalised sweating that involves the whole body, this condition causes visible sweat to appear specifically on the forehead, cheeks, upper lip and hairline—often without any obvious cause such as exercise or hot weather.
Craniofacial hyperhidrosis can have a significant impact on quality of life, making effective management and access to NHS care important. This page focuses specifically on face and scalp sweating rather than sweating from the armpits, palms or soles. While those areas are commonly affected by hyperhidrosis, craniofacial sweating presents unique challenges because it is so visible to others and difficult to conceal.
The NHS recognises craniofacial hyperhidrosis as a genuine medical condition that can be extremely distressing both socially and professionally. Many patients are told it is “just sweating” or that they are simply nervous, but this dismisses the very real impact on daily activities, work performance and personal relationships. There are defined diagnostic criteria and a range of treatment options available.
If you have been struggling with facial or scalp sweating, you are not alone. The condition affects both men and women, can begin at any age, and responds to treatment in the majority of cases. Mr Marco Scarci is a consultant thoracic surgeon in London with a special interest in the surgical management of severe hyperhidrosis, including craniofacial cases where appropriate. His expertise becomes relevant for patients who have exhausted other treatment options and are considering endoscopic thoracic sympathectomy.
Help is available, and the first step is understanding what you are dealing with.
NHS Access and Stepped Approach to Treatment
The NHS employs a stepped approach to treat craniofacial hyperhidrosis, starting from self-care and progressing to specialist treatments for severe cases. Access to some treatments, such as Botox or surgery, can be restricted based on severity or require individual funding requests, and NHS commissioners may limit access due to budget constraints. Typically, first-line management includes strong antiperspirants containing aluminium chloride hexahydrate, followed by specialist options like topical glycopyrrolate cream, oral medications (such as oxybutynin or propantheline bromide), and, in selected cases, botulinum toxin injections or iontophoresis. Referrals for advanced treatments may require an Individual Funding Request (IFR) in certain regions, and not all treatments are available in every NHS trust.

What is craniofacial hyperhidrosis?
Craniofacial hyperhidrosis is a type of excessive sweating that affects the face and scalp. The term “craniofacial” simply refers to the head and face region. Craniofacial hyperhidrosis describes overactivity of the sweat glands in this area, causing sweating excessively beyond what the body needs for temperature control.
People with this condition typically notice visible beads of sweat on the forehead, upper lip, nose, cheeks, scalp and hairline—even when sitting in a cool room or at rest. The sweating often occurs symmetrically, affecting both sides of the face equally, and may be triggered by situations that would not normally cause sweating in most people.
Sweating is part of the body’s normal thermoregulation system, helping to cool the skin when body temperature rises. In hyperhidrosis, however, the sweat glands become overactive without an appropriate trigger. The sympathetic nervous system, which controls the “fight or flight” response, sends excessive signals to these glands even in calm or cool conditions.
Hyperhidrosis affects the water-producing eccrine sweat glands, not the apocrine sweat glands which produce odour. Excessive sweating does not usually cause a bad smell, but harmless skin bacteria can build up and cause an unpleasant smell.
It is important to distinguish between the two main types:
Primary craniofacial hyperhidrosis: No underlying medical cause is found. Sweating is focal (limited to specific areas), symmetrical, occurs at least weekly, impairs daily activities, started before age 25 in most cases, and there may be a family history. It is often present for six months or longer.
Secondary hyperhidrosis: Sweating is caused by another condition such as thyroid disease, diabetes, hormonal conditions like menopause, infections, obesity, or certain medicines. Night sweats or sweating affecting the whole body are more common in secondary cases.
Craniofacial hyperhidrosis is classified as a type of focal hyperhidrosis in NHS and dermatology guidelines. It often starts in adolescence or early adulthood, though some patients first notice symptoms in their 30s or 40s. Both men and women are affected, and the condition can run in families.
Symptoms and daily impact
Facial and scalp sweating can feel fundamentally different from sweating in the armpits or on clammy palms because it is so visible to others. There is nowhere to hide, and patients often describe feeling that everyone is staring at them.
Common symptoms include:
Dripping sweat from the forehead during normal conversation
Sweat running into the eyes, causing stinging and blurred vision. Excessive sweating can cause visible sweat, wet clothes, and clammy palms, it can increase the risk of fungal infections.
Glasses slipping repeatedly due to moisture on the nose and temples
Makeup washing off within minutes of application
Visible damp patches on the hairline, collar or neckline
Wet clothes around the neck even in a cool environment
Hair becoming soaked and lank, particularly around the temples
The sweating usually affects both sides of the face and scalp equally. It may occur with minimal exertion—sometimes just walking into a room or thinking about an upcoming meeting is enough to trigger an episode.
Symptoms often worsen with emotional triggers. Presentations at work, social gatherings, job interviews, and public speaking commonly cause severe episodes. Even pleasant events like weddings or family celebrations can become sources of anxiety.
Psychological impacts:
Embarrassment and fear of being judged
Tendency to avoid photographs or social contact altogether
Reduced confidence at work
Strained relationships when a partner does not fully understand the condition
Crucially, anxiety about sweating can itself trigger more sweating. Many patients describe this vicious cycle in clinic—worrying about whether they will sweat makes them sweat more, which increases the anxiety further. This pattern can be exhausting and demoralising.
When to seek NHS medical advice
You do not need to “just live with” facial or scalp sweating. NHS help is available, and the starting point is your GP.
See your GP if you experience:
Sweating of the face or scalp that is frequent, severe, or interferes with work, driving, reading, or social life
Sweating that seems to happen without any obvious trigger
Episodes that occur several times a week and affect your quality of life
Sweating that started suddenly in adulthood or affects the whole body
Night sweats that soak your bedding
Associated symptoms such as unexplained weight loss, palpitations, tremor, fever, excessive thirst, or passing urine more often than usual
Seek urgent or same-day NHS care (111 or A&E) if excessive sweating is accompanied by:
Chest pain or tightness
Shortness of breath
Confusion or altered consciousness
Very high fever
At your GP appointment, expect a detailed history to be taken. The doctor will ask when the sweating started, which areas are affected, how often it happens, and whether it interferes with daily activities. They will examine your skin and check for signs of thyroid, hormonal or infectious problems. Blood tests may be ordered—for example, thyroid function tests, blood glucose and a full blood count.
If no obvious cause is found and the sweating is focal to the head and face, your GP may diagnose primary craniofacial hyperhidrosis. They can then discuss treatment options or refer you to a dermatologist or specialist hyperhidrosis clinic.
Causes and triggers of craniofacial sweating
In most people with craniofacial hyperhidrosis, no single cause is found. The condition appears to result from a combination of factors rather than a specific underlying disease.
The main mechanisms involved include overactivity of the sympathetic nerves that control sweat glands, a genetic tendency in some families (family history is present in 30-50% of cases), and a heightened stress response that activates sweating even in non-threatening situations. The sweat glands themselves are normal in number and structure—they simply receive too many signals to produce sweat.
Primary craniofacial hyperhidrosis is characterised by:
Long-standing symptoms, often starting in the teens or 20s
Focal sweating affecting the face and scalp specifically
No other illness identified on investigation
Symmetrical distribution
Possible family history
Secondary craniofacial hyperhidrosis may be linked to:
Overactive thyroid
Menopause and other hormonal conditions
Infections
Obesity
Certain medicines, including some antidepressants (excessive sweating can occur as a side effect of these medications)
Low blood sugar
Neurological conditions
Common everyday triggers that patients recognise include:
Heat and humidity
Hot drinks
Spicy food
Alcohol
Strong emotions (excitement, embarrassment, stress)
Caffeine
Sudden temperature changes, such as coming in from cold to a warm room
Some people experience facial flushing along with sweating. This combination can be mistaken for rosacea or menopausal hot flushes, which is why a thorough assessment by a healthcare professional is important for accurate diagnosis.
Self-care and lifestyle measures (NHS-style advice)
Lifestyle changes alone may not cure craniofacial hyperhidrosis, but they can reduce the frequency of episodes and improve your confidence in managing the condition.
Recommended Self-Care Actions
Lifestyle advice for managing hyperhidrosis includes identifying and avoiding triggers such as caffeine, spicy foods, and alcohol.
Antiperspirant use: Use strong antiperspirants (not just deodorant) containing aluminium chloride on the hairline and forehead, applied to cool, dry skin at night.
Face care: Carry a small clean towel, blotting papers or tissues to gently pat the face dry rather than wiping repeatedly.
Hair management: Keep hair shorter or styled away from the forehead and neck to allow evaporation and reduce visible damp patches.
Sweat shields: Consider sweat shields for clothing to protect against visible damp patches.
Allow drying time: Allow moisture to absorb before dressing fully after showering.
Clothing and Hygiene Tips
Clothing: Choose light, breathable fabrics and lighter colours around the collar to make visible sweat less obvious. Wear loose fitting clothes that allow air circulation.
Footwear: Use leather shoes or shoes with breathable materials rather than sports shoes made from synthetic materials; avoid nylon socks.
Socks: Change socks twice daily if you also have sweaty feet—wearing socks that absorb moisture can help reduce discomfort and manage sweat.
Hygiene: Soap substitutes and clothing foot powders can help manage harmless skin bacteria and unpleasant smell.
Anxiety Management
Breathing exercises: Basic anxiety-management measures can also help, reflecting NHS mental health guidance.
CBT and self-help: Breathing exercises, CBT-based self-help resources, and apps recommended by the NHS (such as those available through NHS Apps Library) may reduce the anxiety component that triggers sweating.
Pharmacist advice: Your pharmacist can advise on suitable over-the-counter antiperspirants and gentle, skin-friendly cleansing products for the face and scalp.
What to Avoid
Hot drinks and spicy food: Try to avoid very hot drinks, strong coffee and spicy meals just before stressful events.
Heavy makeup: Avoid heavy, occlusive makeup that traps heat—opt for lighter, oil-free products and setting powders.
Tight headwear: Avoid tight hats, helmets or head coverings for long periods where alternatives are possible.
Alcohol and caffeine: Avoid alcohol and caffeine before important events.
If persistent anxiety is affecting your quality of life, discuss this with your GP—talking therapies and, in some cases, taking medicine like beta blockers may be appropriate.

NHS treatment options for craniofacial hyperhidrosis
Treatment within the NHS typically follows a stepwise approach, starting with the least invasive options and progressing if initial measures are not effective.
Topical treatments
Specialist options include topical glycopyrrolate cream for the face and oral medications like oxybutynin or propantheline bromide, which are used off-label.
Prescription-strength aluminium chloride antiperspirants are usually the first medical treatment offered. These are applied at night to dry skin on the hairline, forehead and upper lip, then washed off in the morning. Initial application is typically for 3-5 consecutive nights, then reduced to once or twice weekly for maintenance. Topical preparations containing aluminium chloride hexahydrate are commonly used and can be applied to the affected areas at night.
Possible side effects include skin irritation and a burning sensation. Using a moisturiser, reducing application frequency, and allowing the skin to be completely dry before application can help minimise these effects. Hydrocortisone 1% cream may be prescribed for up to two weeks if irritation occurs. For those considering treatment options, it’s important to be aware of the real cost of private cancer treatment in the UK, as financial planning can be an essential part of your healthcare journey.
Topical glycopyrrolate (often as a 2% cream) is another option, particularly effective for facial hyperhidrosis. A 2015 systematic review found 96% efficacy with minimal side effects. This is usually prescribed in secondary care.
Oral medications
If topical treatments do not provide adequate relief, oral anticholinergic tablets may be considered. Options include:
Oxybutynin: Shows 80-100% efficacy in studies
Propantheline: Typically 15mg three times daily before meals, up to 120mg daily
Glycopyrronium bromide: Another antimuscarinic option
These medicines work by blocking certain nerve signals that trigger sweating. Common side effects include dry mouth, constipation, blurred vision, photophobia (sensitivity to light), dry skin and urinary retention. They require supervision by your GP or specialist.
Botulinum toxin injections
Botulinum toxin (Botox) injections can be highly effective for craniofacial hyperhidrosis. Tiny injections into the forehead or scalp temporarily block the nerves that trigger sweat glands.
Key points about Botox treatment:
Efficacy of 70-100% reported in studies
Effects typically last 4-6 months
Repeat injections are needed 2-3 times yearly
Possible minor and transient side effects include brow asymmetry or mild forehead muscle weakness
NHS availability is variable and subject to local commissioning policies
A 2022 study comparing topical glycopyrrolate and botulinum toxin found complete response in 75% of patients with both treatments, though botulinum effects lasted longer (up to 6 months).
Other treatments
Additional options sometimes offered in specialist units include:
Iontophoresis: Uses a weak electric current passed through a wet pad to reduce sweating; more commonly used for palms and soles but can be adapted for facial areas
Beta blockers: May help selected patients where anxiety and flushing are strong triggers
Oral beta blockers require medical supervision and careful monitoring
Not every hospital trust offers all treatments. Referral to dermatology or a specialist hyperhidrosis service may be required for advanced options. Your GP can explain the local pathway and refer you appropriately.
Surgical options and the role of thoracic surgery
Surgery is rarely the first treatment option and is reserved for carefully selected patients with severe hyperhidrosis that has not responded to other treatments. Before surgery is considered, patients should have tried and documented failure of conservative measures, topical treatments and usually oral medications or botulinum toxin.
Endoscopic Thoracic Sympathectomy (ETS) is considered a last resort for severe cases, involving cutting the nerves responsible for sweating.
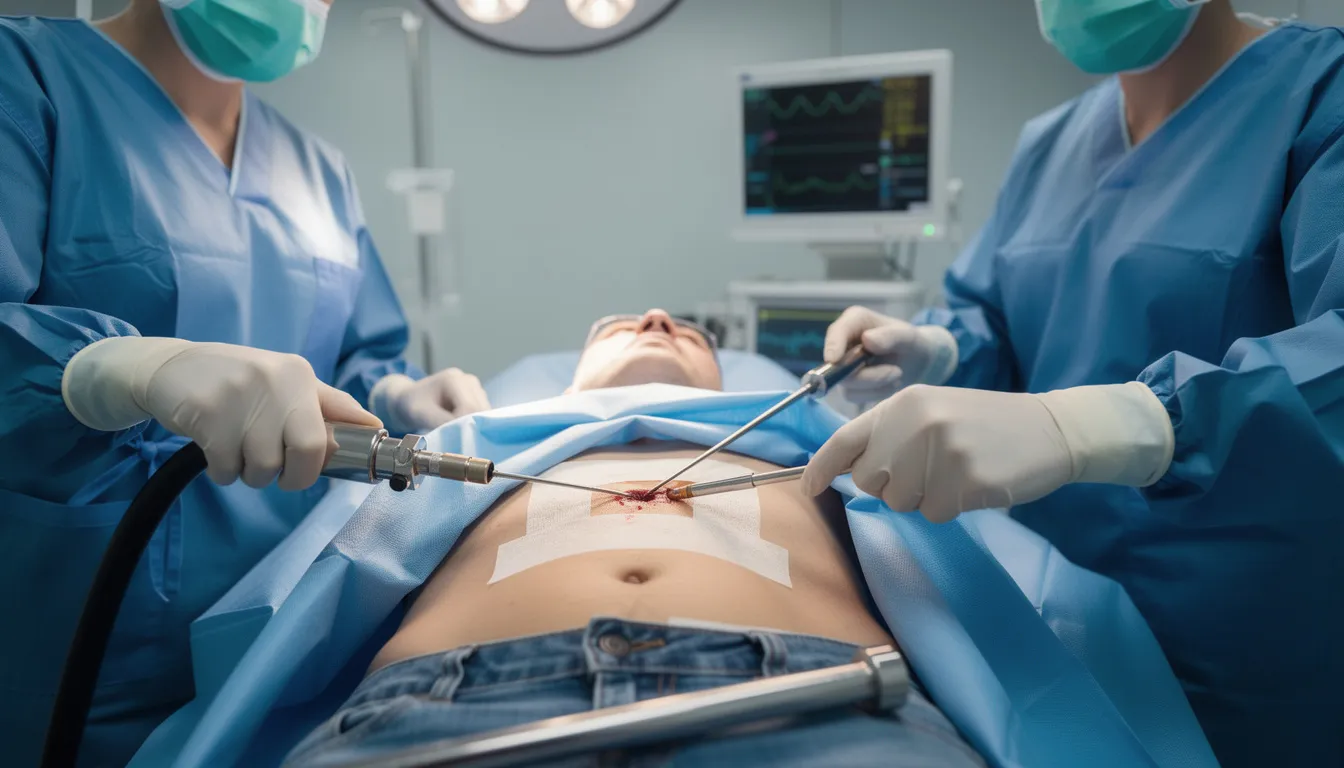
Endoscopic thoracic sympathectomy (ETS)
Endoscopic thoracic sympathectomy is a keyhole operation performed inside the chest. The surgeon interrupts part of the sympathetic nerve chain that drives sweating. The procedure is typically performed under general anaesthetic using minimally invasive techniques, usually requiring just small incisions.
ETS is more commonly performed for palmar (hand) and axillary (armpit) hyperhidrosis, but it may be considered in selected craniofacial cases—particularly sweating affecting the forehead and upper face.
Potential benefits:
High efficacy: 70-100% success rate in studies with mean 29-month follow-up
Low recurrence rate: 0-8% in most series
Immediate or near-immediate effect on sweating
Potential risks and complications:
Compensatory sweating: Increased sweating on the trunk, back or legs, which can be troublesome in some patients
Pneumothorax (collapsed lung): Occurs in 0-1% of cases, usually resolves without major intervention
Infection
Horner’s syndrome (very rare when operating for facial sweating): drooping eyelid and constricted pupil on one side
NHS access to ETS is limited and usually requires referral from a dermatologist or other specialist. Strict criteria apply, and thorough consent is essential.
Mr Marco Scarci’s expertise
Mr Marco Scarci is a consultant thoracic surgeon in London with extensive experience in minimally invasive thoracic procedures. He offers surgical assessment for patients with severe hyperhidrosis, including craniofacial cases where surgery is being considered after other options have failed.
His approach uses keyhole techniques to minimise hospital stay and recovery time. Patients considering surgery should expect a detailed discussion of non-surgical alternatives, realistic expectations, and potential long-term effects before any procedure is recommended.
Surgery is not suitable for everyone, and Mr Scarci works with patients to determine whether ETS is appropriate based on their individual circumstances, severity of symptoms, and response to previous treatments.
Private versus NHS pathways with Mr Marco Scarci
Most patients with craniofacial hyperhidrosis will start on the NHS pathway through their GP. However, some choose private consultation to be seen more quickly, access a wider range of options, or discuss surgical assessment earlier in their journey.
The NHS pathway
A typical NHS journey for craniofacial hyperhidrosis follows these steps:
GP assessment: History, examination, blood tests if indicated, diagnosis of primary vs secondary hyperhidrosis
Initial treatments: Lifestyle advice, prescription-strength aluminium chloride, possibly oral anticholinergics
Referral to dermatology: If first-line treatments are ineffective after 3-6 months
Specialist treatments: Botulinum toxin, topical glycopyrrolate, iontophoresis where available
Onward referral to thoracic surgery: In selected severe cases where ETS is being considered
Wait times vary by region, and not all treatments are available in every area. Your GP can explain local commissioning arrangements.
Private consultation with Mr Scarci
Private consultations offer:
Face-to-face and virtual appointments available in London
Shorter waiting times for initial assessment
Comprehensive review of previous investigations and treatments
Detailed discussion of whether thoracic surgery is appropriate, or whether further dermatology or medical management is advisable first
Access to patients from the UK and overseas
Mr Scarci uses minimally invasive keyhole techniques where surgery is indicated, aiming to reduce hospital stay and recovery time while maximising safety.
Patients can move between NHS and private pathways in line with NHS rules. The goal in both settings is safe, evidence-based care tailored to individual needs and circumstances.
Living with craniofacial hyperhidrosis
Practical Coping Strategies
Living with visible facial sweating can be emotionally challenging. Many patients describe years of embarrassment before seeking help, and some have adjusted their entire lives around the condition—avoiding social events, turning down promotions, or wearing only certain colours.
Plan ahead: Plan ahead for important events by allowing extra time to cool down and compose yourself.
Be prepared: Keep spare clothing, a small towel or facial wipes, and makeup or grooming items in a bag or at your workplace.
Choose seating wisely: Choose seating near windows, air conditioning vents, or cooler areas when possible.
Portable fan: Carry a portable fan for discreet cooling.
Cool water: Use cool water on your wrists and temples before entering stressful situations.
Mental Health Support
Feelings of embarrassment and social anxiety are common and completely understandable. You are not overreacting, and your distress is valid.
NHS talking therapies (IAPT services in England or equivalent local services) can help with anxiety linked to hyperhidrosis. Cognitive behavioural therapy (CBT) is particularly useful for breaking the cycle where anxiety about sweating triggers more sweating.
The International Hyperhidrosis Society provides reliable information and support. Your GP can provide a patient information leaflet about hyperhidrosis and direct you to appropriate local resources.
Consider involving close family or friends so they understand the condition is medical and not simply due to “nervousness.” Having people around you who understand can reduce the isolation that many patients feel.
The removal of stigma starts with recognising that hyperhidrosis is a genuine medical condition, not a personal failing.
Frequently asked questions
Is craniofacial hyperhidrosis dangerous or a sign of something serious?
Primary craniofacial hyperhidrosis is not dangerous and is not usually a sign of serious underlying disease. However, if your sweating started suddenly, affects the whole body, or is accompanied by other symptoms, your GP should exclude secondary causes such as thyroid problems or hormonal conditions. The sweating itself is distressing but medically harmless.
Can craniofacial hyperhidrosis go away on its own with age?
Some patients report improvement in their 30s or 40s, but for many the condition persists throughout life. It is not something you should simply wait out—effective treatments are available, and there is no reason to suffer unnecessarily.
Are there specific NHS guidelines for treating facial and scalp sweating?
NHS guidelines for hyperhidrosis apply to all focal types, including craniofacial. Treatment follows a stepwise approach: lifestyle measures first, then topical antiperspirants, oral anticholinergics, botulinum toxin, and finally surgery in selected cases. Severity is often assessed using the Hyperhidrosis Disease Severity Scale (HDSS).
Can I still exercise if I have severe facial sweating?
Yes, exercise is important for overall health and should not be avoided. Many patients find that regular exercise actually helps regulate their sweating over time. Choose cooler times of day, exercise in air-conditioned environments where possible, and keep cool water and a towel nearby.
Will shaving my head or changing my hairstyle really make a difference?
Shorter hair or styles that keep hair away from the forehead and neck can allow sweat to evaporate more easily, reducing the visible wet appearance. This is not a cure but can help with management and confidence.
What happens at my first appointment with a specialist?
A specialist will take a detailed history, examine the affected areas, and review any previous treatments you have tried. They may ask you to demonstrate which areas sweat most and how this affects your life. Discussion will cover what further treatment options are available and appropriate for your situation.
How successful is surgery for craniofacial hyperhidrosis and who is it suitable for?
ETS shows success rates of 70-100% for reducing sweating, with low recurrence. However, it carries a risk of compensatory sweating elsewhere on the body. Surgery is generally reserved for patients who have tried and failed other treatments, and requires careful discussion of risks and realistic expectations. Mr Scarci assesses each patient individually to determine suitability.
References, review dates and next steps
This article is based on current evidence and UK/NHS guidance on hyperhidrosis and focal craniofacial sweating, including recommendations from NHS Scotland and NHS England pathways, British Association of Dermatologists guidelines, and published systematic reviews.
Page last reviewed: January 2025 | Next review due: January 2028
For a comprehensive overview of excessive sweating and available therapies, see our hyperhidrosis treatment guide.
Your next steps:
Speak to your GP for personalised NHS advice and to rule out secondary causes
Consider asking for referral to dermatology or a hyperhidrosis clinic if current measures are not working
Contact Mr Marco Scarci’s team if you wish to explore specialist thoracic surgical assessment for severe, refractory hyperhidrosis
You do not have to manage this condition alone. Whether you are just starting to seek help or have exhausted other options, effective treatment pathways exist—and the right support can make a real difference to your quality of life.