That sudden, sharp stab of chest pain, followed by a frustrating inability to catch your breath, is a genuinely frightening experience. It immediately makes you question what's going on. One possibility is a pneumothorax, commonly known as a collapsed lung, and recognising the symptoms is the first crucial step towards getting the right treatment. The most important thing to do is get medical help straight away; a quick diagnosis is key to a good outcome.
Recognising the Signs of a Collapsed Lung
So, what exactly is a collapsed lung? Imagine the space between your lung and your chest wall – the pleural space. It's meant to be a thin, lubricated area that lets your lungs move freely. A pneumothorax occurs when air somehow gets into that space, putting pressure on the outside of your lung and causing it to deflate, either partially or fully.
This isn't always caused by a dramatic injury. A primary spontaneous pneumothorax can happen out of the blue, for no clear reason, and is surprisingly common in tall, thin young men. On the other hand, a secondary spontaneous pneumothorax happens as a complication of an underlying lung disease, like COPD or cystic fibrosis.
Common Symptoms to Watch For
The signs can appear without any warning at all. You could just be going about your day when you're suddenly hit with a sharp, one-sided chest pain. That’s a hallmark symptom.
Keep an eye out for these classic indicators:
- Sudden, sharp chest pain, which often feels worse when you try to take a deep breath or cough.
- Shortness of breath (dyspnoea) that can feel mild or become quite severe, depending on how much of the lung has collapsed.
- A distinct feeling of tightness in your chest.
- A rapid heart rate as your body works overtime to compensate for the lower oxygen levels.
A collapsed lung isn't just a minor blip. It's a serious medical event that compromises your body's ability to get the oxygen it needs. Trying to "wait it out" can lead to much bigger problems, which is why acting fast is so critical.
Why You Must Act Quickly
While a collapsed lung sounds like a rare event, it's actually becoming more common. Studies have shown that hospital admissions for spontaneous pneumothorax in England shot up by 55% between 1968 and 2016. Notably, 73% of these cases were in men. This trend underlines just how important it is for people to be aware of the signs. You can find more details in this study on pneumothorax trends.
This flowchart breaks down the decision process in the simplest terms.
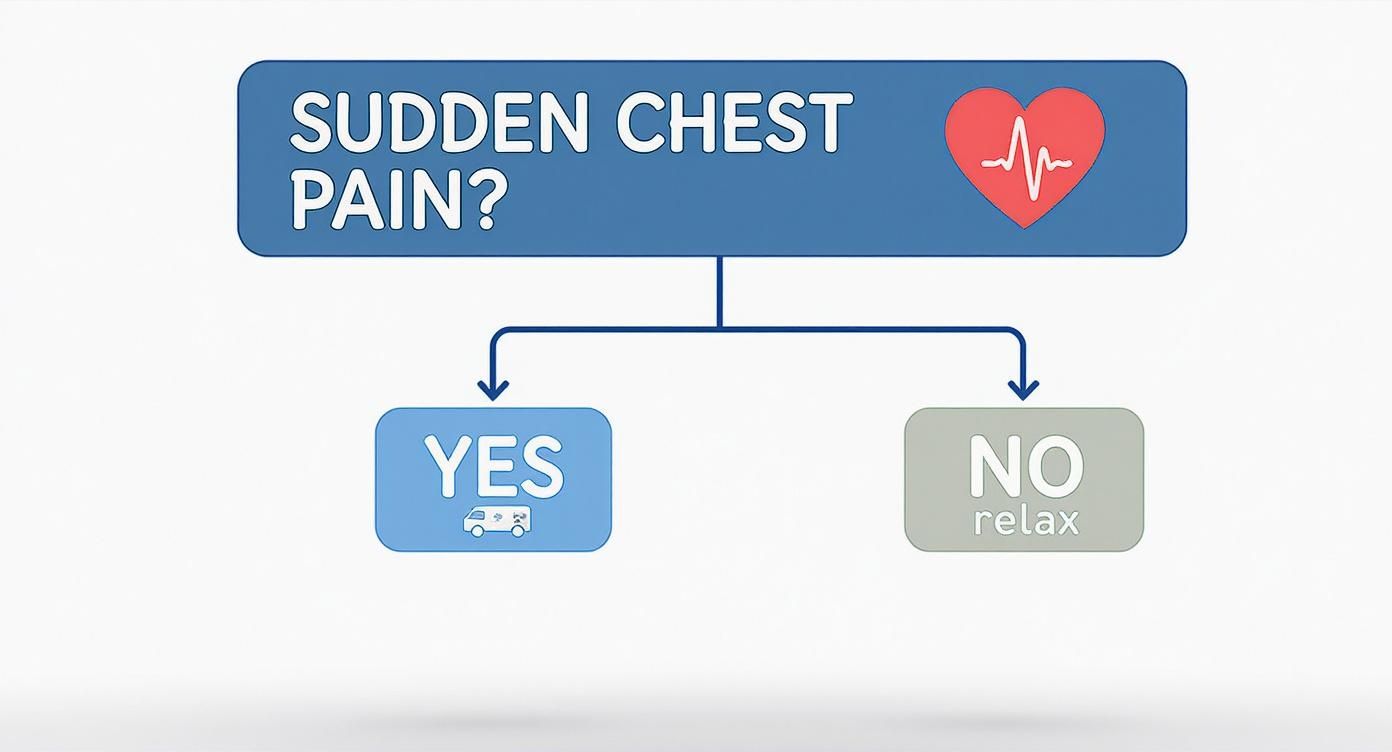
The message couldn't be clearer: if you experience sudden, unexplained chest pain, you need to call for an ambulance. It is always better to get it checked out and find it’s nothing serious than to delay treatment for a condition like a pneumothorax. Getting to grips with the potential causes, complications, and management of pneumothorax can help you feel more in control and make smart decisions about your care.
Pneumothorax Treatment Pathways at a Glance
Once you're at the hospital, the team will assess the size of the pneumothorax and how it's affecting you. The treatment path they choose depends heavily on these factors. Here's a quick overview of the main options.
| Treatment Approach | Best For | Goal of Treatment |
|---|---|---|
| Observation | Very small collapses (<2 cm) in stable patients with minimal symptoms. | Allow the air to be reabsorbed by the body naturally over time. |
| Needle Aspiration | Small to moderate collapses in stable patients as a first intervention. | Manually draw the air out of the pleural space with a needle and syringe. |
| Chest Drain | Larger collapses (>2 cm) or for patients who are breathless or unstable. | Insert a tube to continuously drain the air and allow the lung to re-inflate. |
| Surgery (VATS) | Recurrent collapses or when the lung fails to re-inflate with a drain. | Permanently fix the problem by removing weak areas of the lung and/or making the lung stick to the chest wall (pleurodesis). |
This table is just a guide, of course. Your specialist will always recommend the best course of action for your specific situation, taking your overall health and the specifics of the collapse into account.
What to Expect at the Hospital

Arriving at A&E feeling breathless and in pain is a daunting experience. Knowing what the medical team will do can help ease some of that stress. Their immediate priority is to work out if you have a collapsed lung and, crucially, how serious it is.
The assessment will be quick and to the point. Doctors and nurses will check your vital signs—your heart rate, breathing, and oxygen levels (with a small, painless clip on your finger). They’ll also listen carefully to your chest with a stethoscope, searching for subtle changes in your breath sounds that point to trapped air outside the lung. This hands-on check gives them a very good initial idea of what’s going on.
Getting a Clear Picture with Imaging
The gold standard for confirming a pneumothorax is a chest X-ray. It’s a fast and simple test that gives the team a clear view of the air in your pleural space, allowing them to see exactly how much the lung has deflated. On the image, this trapped air shows up as a dark patch next to the fine white line marking the edge of your collapsed lung.
A key part of the assessment is measuring the size of the collapse. Following UK guidelines, the doctor measures the distance from the edge of the lung to the inside of your chest wall.
- A small pneumothorax is one where this gap is less than 2 cm.
- A large pneumothorax is when the gap is 2 cm or more.
This measurement is fundamental, as it heavily influences the treatment plan. A small collapse in someone who feels relatively well might just need careful monitoring, while a large one almost always requires a procedure to remove the air.
It's worth remembering that the X-ray is just one piece of the puzzle. Your doctor will always consider the size of the collapse in the context of your symptoms. Someone with a large pneumothorax who isn’t breathless might be managed differently from another person with a small one who is in severe distress.
Medical Terms You Might Hear
During the diagnosis, you may hear the term tension pneumothorax. This is a specific and very serious type of collapsed lung where air gets trapped and builds up under pressure. It's a medical emergency because the pressure can squash the heart and major blood vessels, stopping them from working properly. It's diagnosed by clinical signs—like severe breathlessness and dangerously low blood pressure—not just from the X-ray.
When a CT Scan is Necessary
Sometimes, a chest X-ray doesn’t tell the whole story. Your consultant might arrange for a Computerised Tomography (CT) scan if they need more detail. This is often the case when:
- The reason for the pneumothorax isn't obvious.
- They suspect an underlying lung condition, such as emphysema.
- They are looking for the root cause, like tiny air blisters (bullae or blebs) on the lung’s surface, which are common culprits in spontaneous pneumothorax.
A CT scan creates a highly detailed, 3D-like image of your chest, giving your specialist a comprehensive view. This information is vital for planning the best long-term treatment and figuring out how to stop it from happening again. Getting this complete diagnostic picture ensures your treatment plan is perfectly suited to your individual situation.
Exploring Non-Surgical Treatment Options

When you're told you have a collapsed lung, it’s easy to assume that surgery is the only answer. But that’s often not the case, especially if it’s your first time experiencing a spontaneous pneumothorax. The initial goal is quite simple: get the trapped air out of the space around your lung so it can expand properly and start healing.
The path we take depends almost entirely on two things: the size of the collapse we see on your X-ray and, just as importantly, how breathless you feel. For many people, a non-surgical approach is the first and most effective step.
Conservative Management: When Less Is More
If you have a very small pneumothorax and you’re not feeling too short of breath, the best treatment might be the simplest one of all: observation. We often call this conservative or 'expectant' management. It's essentially a "watch and wait" strategy.
Your body is surprisingly good at healing itself. It can naturally reabsorb the trapped air from the pleural space, typically at a rate of about 1.25% of the chest cavity's volume each day. During this time, we'll monitor you closely and often give you some supplemental oxygen, which helps speed up that absorption process and keeps your blood oxygen levels stable.
This approach is perfect for patients who are otherwise healthy with minimal symptoms. It avoids any invasive procedures, but it does require a bit of patience and follow-up X-rays to make sure the lung is slowly re-inflating as expected.
Needle Aspiration: A Simple First Intervention
If the pneumothorax is larger, or if it's making you noticeably breathless, we often move on to needle aspiration. This is a very straightforward procedure that provides much more immediate relief by manually drawing the air out.
Think of it like letting air out of a tyre. After numbing a small patch of skin on the front of your chest with local anaesthetic, we carefully guide a thin needle connected to a syringe into the pleural space.
As we gently draw the air out, you might feel a strange bubbling or releasing sensation. Many patients find their breathing gets easier almost instantly. We repeat this until we can't get any more air out, which is a great sign that the lung has re-expanded.
For a first-time primary spontaneous pneumothorax that's on the larger side but isn't causing severe distress, needle aspiration is often our go-to. It's quick, minimally invasive, and can often be done right in the emergency department, sometimes preventing a hospital admission altogether.
It’s worth noting, however, that treatment philosophies can differ. A survey of 100 UK respiratory specialists revealed that only 51% would choose conservative management for a large but minimally symptomatic pneumothorax. This highlights that more traditional interventions like aspiration or even chest drains are still widely used, even as modern guidelines shift to focus more on how the patient feels rather than just the size of the collapse.
When a Chest Drain Is Necessary
What if needle aspiration doesn't quite do the trick, or the lung collapses again soon after? In that case, the next step is usually a chest drain. This is also the standard treatment for very large collapses, those caused by an injury, or for patients with underlying lung conditions.
A chest drain (or chest tube) is a small, flexible plastic tube that we insert through the chest wall into the pleural space. This is always done under local anaesthetic to make you as comfortable as possible. The tube is then connected to a special one-way valve system that lets air out of your chest but won't let any back in.
This continuous drainage gives your lung the chance to fully re-inflate and, crucially, stay inflated while the tear that caused the leak heals. This usually means a hospital stay of a few days, with regular X-rays to track your progress.
Comparing Minimally Invasive Pneumothorax Procedures
To help you understand the common non-surgical options at a glance, this table breaks down what each procedure involves and who it's typically for.
| Procedure | Typical Patient | Procedure Overview | Hospital Stay |
|---|---|---|---|
| Observation | Small pneumothorax, minimal symptoms, otherwise healthy. | Monitoring with oxygen and follow-up X-rays to allow the lung to heal naturally. | May be managed as an outpatient or require a short admission for monitoring. |
| Needle Aspiration | Medium to large pneumothorax with mild to moderate breathlessness. | A needle and syringe are used to manually withdraw trapped air from the pleural space under local anaesthetic. | Often done in A&E; may avoid admission if successful, or require a 24-hour stay. |
| Chest Drain | Large/symptomatic pneumothorax, failed aspiration, or secondary pneumothorax. | A small tube is inserted into the chest to continuously drain air via a one-way valve system. | Requires hospital admission, typically for a few days, until the air leak has sealed. |
Each of these methods is designed to resolve the immediate problem—the collapsed lung—with the least intervention necessary.
Ambulatory Care: Going Home with a Drain
In the past, a chest drain meant being stuck in a hospital bed, connected to a large, bubbling water-seal bottle. Thankfully, things have moved on, and we now have ambulatory devices that offer much more freedom.
For the right patient, we can attach a small, portable one-way device called a Heimlich valve to the chest drain. This compact valve lets you move around easily and, in many cases, even allows you to go home while your lung continues to heal. The benefits are significant:
- Greater Comfort: There's nothing quite like recovering in your own bed.
- Reduced Risk: It minimises your time in hospital, lowering the risk of picking up an infection.
- Increased Mobility: Being able to walk around and manage light daily activities can actually help your recovery.
Despite these clear advantages, that same UK survey found that only 19% of specialists reported using ambulatory devices. This shows that this excellent, patient-friendly option is still underused in many centres. When discussing your care, it's always a good idea to explore the full range of alternatives to surgery for thoracic conditions with your specialist to see if an ambulatory approach could be right for you.
Deciding if Surgery Is the Right Path for You
https://www.youtube.com/embed/rggmkd1C5UQ
While we often try non-surgical treatments first, they don't always offer a permanent fix. If you've had a collapsed lung before, the worry of it happening again can hang over your head. This is where we start talking about surgery. It’s a definitive way to fix the underlying problem and dramatically lower the chances of it coming back.
The decision to recommend surgery is never made lightly. Your specialist will usually bring it up as the best path forward if you find yourself in one of a few specific situations.
When Is Surgery Recommended?
We generally suggest surgery when there's a clear pattern of recurrence or when the initial, less invasive treatments just haven't done the job.
There are a few key signs that point towards a surgical solution:
- It’s Happened Before: If you’ve already had one pneumothorax, your risk of another is unfortunately quite high. A second collapse is a strong signal that we need to intervene surgically to prevent a third or fourth.
- A Persistent Air Leak: Sometimes, even after a chest drain is in and the lung is back up, the small tear that caused the problem refuses to heal. If air keeps leaking for more than a few days, it’s time to go in, find the source, and seal it for good.
- You Work in a High-Risk Profession: For some people, a sudden collapsed lung could be truly catastrophic. If you're a pilot, a professional diver, or someone who works in a remote area, we often advise definitive surgery even after a first episode, just to eliminate that risk.
The goal here isn’t just to re-inflate the lung for now—it's to stop it from ever collapsing again. This gives you the peace of mind to get back to your life without that constant worry.
Introducing Video-Assisted Thoracoscopic Surgery (VATS)
The thought of chest surgery can be daunting, but the reality is a world away from the large, open operations of the past. Today, the standard is Video-Assisted Thoracoscopic Surgery (VATS), a minimally invasive technique that has completely changed how we treat a collapsed lung.
Instead of one large incision, a VATS procedure involves making just a few small 'keyhole' cuts. We insert a tiny high-definition camera and specialised instruments through these ports, which gives us a crystal-clear, magnified view of your lung on a monitor. It allows for incredibly precise surgery without the major trauma of opening up the chest wall.
The benefits of VATS over traditional open surgery are huge. Patients experience far less pain, have a much shorter hospital stay—often just a few days—and are able to get back to their normal lives much, much faster.
Take, for example, a case study of a 21-year-old man who had two collapsed lungs. A VATS procedure was the definitive answer. Using this keyhole technique, surgeons were able to find and remove the weak air sacs causing the trouble and perform a second procedure to make sure the lung stayed up permanently. You can read the full details of this successful pneumothorax treatment and see how it prevented any further episodes.
What Happens During VATS for Pneumothorax?
The VATS procedure for pneumothorax usually combines two key steps in one operation to give you the best possible long-term result.
First, the surgeon has to deal with what caused the collapse in the first place.
1. Bullectomy or Stapling
In most spontaneous pneumothorax cases, the culprits are small, weak air blisters on the lung's surface, known as bullae or blebs. During VATS, the surgeon can easily spot these weak areas and remove them with a special surgical stapler. This gets rid of the source of the leak.
2. Pleurodesis
With the bullae gone, the next step is to stop the lung from collapsing again. We do this with a technique called pleurodesis, which is designed to make the lung stick to the inside of the chest wall. This completely eliminates the potential space where air could collect in the future.
There are a couple of ways we can achieve this:
- Mechanical Pleurodesis: The surgeon uses a small, dry gauze pad to gently abrade the lining of the chest wall (the pleura). This causes a mild, controlled inflammation that makes the lung surface adhere to the chest wall as it heals.
- Talc Pleurodesis: In some situations, a sterile medical-grade talc powder is puffed into the chest cavity. This triggers a stronger inflammatory response, which creates a very tough and reliable adhesion.
By combining these techniques, VATS provides a durable, long-term solution. Studies show it cuts the risk of another collapsed lung down to less than 5%. Deciding on surgery is a big step, but knowing that modern, minimally invasive options like VATS exist can make that decision feel much less intimidating and a lot more hopeful.
Your Recovery Roadmap and Preventing Recurrence

Leaving the hospital after treatment for a collapsed lung is a huge step, but it’s really just the beginning of the next phase: your recovery. Knowing what to expect and how to protect your lungs moving forward is what allows you to get back to your life with confidence.
Naturally, your personal timeline will hinge on the treatment you received. If your lung was managed with simple observation or a needle aspiration, you can expect a fairly swift recovery. However, if you needed a chest drain or underwent VATS surgery, your body is going to require a bit more time to heal properly.
Managing Pain and Regaining Strength
After any procedure, a degree of discomfort is completely normal. This is especially true following a chest drain or surgery, where the incisions and internal healing can leave you feeling quite sore. Your hospital team will send you home with a clear pain management plan—it's crucial to stick to it. Keeping on top of the pain isn't just about comfort; it enables you to breathe more deeply and move around, both of which are fundamental to a good recovery.
You’ll be encouraged to start gentle walking almost immediately. This simple act is fantastic for preventing complications like blood clots and helps keep your lungs active. The golden rule is to listen to your body, starting small and gradually building up your activity levels over the coming weeks.
Simple breathing exercises are also a cornerstone of recovery. A physiotherapist will often show you specific techniques designed to help fully re-expand your lung and build back the strength in your respiratory muscles. A classic and effective exercise is deep diaphragmatic breathing:
- Find a comfortable position, either sitting or lying down.
- Place one hand on your chest and the other on your stomach.
- Breathe in slowly through your nose, focusing on making your stomach rise more than your chest.
- Then, breathe out slowly through pursed lips, feeling your stomach fall.
Doing this for just a few minutes, several times a day, can make a surprising difference. For a more detailed look at what to expect after an operation, you can find a wealth of practical information on recovering from pneumothorax surgery.
Focusing on Prevention
Once you’ve experienced a pneumothorax, preventing another one becomes the absolute priority. The risk of it happening again after a first episode, particularly if managed conservatively, can be quite high.
For patients who have had a primary spontaneous pneumothorax, the chance of a recurrence is estimated to be between 20-30% within two years if treated with observation or a chest drain alone. In contrast, definitive surgical treatment like VATS with pleurodesis slashes this risk dramatically to less than 5%. You can explore these pneumothorax recurrence statistics in more depth.
The single most important lifestyle change you can make is to stop smoking. Smoking is incredibly damaging to lung tissue and is the number one modifiable risk factor for both an initial collapsed lung and a recurrent one.
Your follow-up appointments are not just a box-ticking exercise; they are essential. During these visits, your specialist will almost certainly order another chest X-ray to get visual confirmation that your lung has remained fully inflated. This is also your time to ask questions and get clear guidance on returning to your normal activities.
Returning to Normal Activities
Patience is a virtue when you’re getting back into your routine. Your consultant will provide specific advice tailored to you, but here are some general guidelines I often give my patients:
- Work: If you have a desk job, you might feel ready to return within one to two weeks. For more physically strenuous jobs, you'll likely need four to six weeks, sometimes longer.
- Driving: You absolutely should not drive while taking strong pain medication. Most people feel comfortable getting back behind the wheel within a week or two of a minor procedure, or a bit longer after surgery.
- Exercise: Gentle exercise like walking can be resumed straight away. However, you must avoid strenuous activities, contact sports, and any heavy lifting for at least a month—and always get the green light from your doctor first.
- Air Travel: This is a big one. The changes in air pressure inside a plane cabin can be risky for a healing lung. As a rule, you should wait at least one week after a follow-up X-ray has confirmed the pneumothorax is completely resolved. Your specialist will give you the final all-clear.
Going through a pneumothorax can be a genuinely frightening experience, but with the right aftercare and preventative measures, you can get back to living your life fully and without constant worry.
Answering Your Questions About Pneumothorax
It’s completely normal to have a million questions running through your head when you’re told you have a collapsed lung. The medical jargon alone can be confusing, and the road ahead might feel uncertain. Let's walk through some of the most common concerns to give you a clearer picture of what to expect.
How Long Will I Be in Hospital?
This really depends on the treatment you need. If you have a very small pneumothorax that can be managed by just keeping an eye on it, you might only be in hospital for 24 to 48 hours for observation.
If a chest drain is needed to help your lung expand again, a hospital stay of a few days is typical. We need to wait until the air leak has fully sealed before the drain can come out. For patients who have keyhole (VATS) surgery, the standard stay is usually between two and five days. It’s also good to know that some people are candidates for modern ambulatory drains, which are small, portable devices that let you go home much sooner.
Can I Fly After a Collapsed Lung?
You’ll definitely need to put any travel plans on hold for a little while. The pressure changes in an aeroplane cabin can be dangerous for a healing lung and could even make it collapse again.
In the UK, the general advice is to wait at least one week after a chest X-ray confirms your lung is fully re-inflated and stable. The risk is much lower if you’ve had a definitive procedure like pleurodesis to prevent it from happening again.
The bottom line: Always get personalised clearance from your specialist before booking any flights. It's just as important to tell your travel insurance provider about your recent medical history to ensure you’re fully covered.
What Are the Chances of This Happening Again?
This is a big worry for many people, and understandably so. If you’ve had a first-time spontaneous pneumothorax that was treated without surgery (just observation or a chest drain), the risk of another one is surprisingly high—up to 30%.
This is where definitive surgery really shines. A procedure like a VATS pleurodesis is incredibly effective at stopping future collapses, dropping the recurrence risk to less than 5%. Outside of surgery, the most powerful thing you can do to lower your risk is to stop smoking.
When Can I Get Back to Exercising?
Easing back into physical activity is the name of the game. You'll actually be encouraged to start moving pretty soon after treatment, with gentle walking and deep breathing exercises to help your recovery along.
You’ll need to steer clear of anything strenuous—that means no heavy lifting, contact sports, or intense workouts for several weeks. Your doctor will give you a specific timeline based on your situation. It's also worth knowing that some high-risk activities, like scuba diving, might be off the table for good because of the extreme pressure changes involved. Always follow your medical team's advice.
It's interesting to see how wider events have shaped treatment, too. UK research highlighted how the COVID-19 pandemic shifted approaches, with admissions hitting a peak in January 2021. The pressure on hospitals pushed for wider adoption of less invasive options, prompting the British Thoracic Society to update its guidelines. The focus moved towards treating the patient's symptoms rather than just the size of the collapse on an X-ray. You can read more about these findings on pneumothorax management for a deeper dive.
Going through a pneumothorax diagnosis can feel overwhelming, but you don’t have to do it alone. For expert guidance and access to advanced, minimally invasive treatments in London, consider a consultation with Marco Scarci Thoracic Surgery. Mr Scarci specialises in providing rapid, patient-focused care to help you recover quickly and with peace of mind. To explore your options for private thoracic care, visit https://marcoscarci.co.uk.
Article created using Outrank