When you're faced with a lung cancer diagnosis, surgery often represents the most direct path to a cure, especially if we've caught the disease in its early stages. The fundamental goal is simple but powerful: to physically remove the tumour and a margin of healthy tissue around it, preventing the cancer from spreading.
Taking that first step to understand what the surgery involves can make a world of difference in how you approach your treatment.
Understanding Your Surgical Treatment Options

Hearing the words "lung cancer" can feel incredibly daunting, but getting a clear picture of your treatment plan is the best way to regain a sense of control. For many of my patients, lung cancer surgery is the cornerstone of their treatment, offering a clear route to removing the disease.
While the primary goal is often to cure the cancer completely, surgery plays a few other vital roles in your care:
- Diagnosis: In some situations, we need to take a small tissue sample (a biopsy) during an operation to get a definitive diagnosis of the cancer type.
- Staging: Surgery helps us understand exactly how far the cancer has spread, which is critical for planning any further treatment you might need.
- Symptom Relief: If a tumour is causing problems like shortness of breath, surgery can be used to remove the blockage and make you more comfortable.
How Staging Shapes Your Surgical Plan
Think of cancer staging as creating a detailed map of the disease. It tells us the size of the tumour, its precise location, and whether it has moved to nearby lymph nodes or other parts of the body. This map is absolutely essential because it determines if surgery is the right choice for you and, if so, which specific operation will be most effective.
As a general rule, surgery offers the best outcomes for early-stage (Stage I and II) non-small cell lung cancer (NSCLC).
"When I was diagnosed, the first thing I worried about was the operation itself. But my surgeon explained that the goal was to remove the cancer completely. Understanding that purpose—that it was about a cure—changed my entire perspective. It gave me a clear focus during a very confusing time." – A Patient's Reflection
The outlook for patients is better than ever. National survival rates in England and Wales are at their highest recorded levels, with one-year survival now at 50% in England and 46% in Wales. Surgery is the main driver behind these high curative treatment rates for early-stage lung cancer. You can read more about the progress in UK lung cancer care.
This guide is designed to walk you through the different types of operations and the modern, minimally invasive techniques we use, giving you a clear and honest overview of what to expect on your journey.
A Patient's Story: David's Journey Through Lung Cancer Surgery
Clinical details and surgical techniques are one thing, but hearing from someone who has actually walked this path can make all the difference. While statistics tell you about outcomes, a personal story brings the hope, resilience, and reality of undergoing lung cancer surgery to life.
I'd like to share the story of one of my patients, David. A fit and active man, his diagnosis came as a complete shock after a persistent cough led his GP to order a chest X-ray. Like for so many others, that initial feeling was one of disbelief and fear.
When David first came to my clinic, he was understandably anxious. We sat down together, went through his scans, and talked through why a robotic-assisted lobectomy offered him the very best chance of a complete cure. My priority was to move things along swiftly, ensuring he and his family felt completely informed.
"The speed of it all was reassuring. From meeting Mr Scarci to being in the hospital was just over a week. You don’t have too much time to dwell on the 'what ifs'. You just focus on the next step, and for me, that was getting the cancer out." – David, Robotic Lobectomy Patient
David’s robotic surgery went exactly as planned. Because we used a minimally invasive approach, his hospital stay was remarkably short—just three days. Six weeks after his operation, the final pathology report confirmed the surgery had removed all the cancer with clear margins. The relief was palpable. Today, he is back to his active lifestyle, enjoying time with his grandchildren, and is living proof that a return to a full and healthy life after lung cancer surgery is not just possible, but an achievable goal.
The Different Types of Lung Resection Surgery

When it comes to lung cancer surgery, there’s no one-size-fits-all approach. The right operation for you will depend on the tumour's size, its precise location, and whether it's contained or has started to spread. Getting to grips with the different procedures can make those initial conversations about your treatment plan feel a lot less daunting.
A simple way to think about it is to picture your lungs as a tree. The right lung has three main limbs (we call them lobes), and the left has two. Each lobe is made up of smaller branches (segments). The type of surgery simply describes how much of this "tree" we need to remove to get rid of the cancer for good.
Wedge Resection: Removing a Small Part of a Lobe
A wedge resection is the most precise and limited type of lung surgery. As the name suggests, the surgeon removes a small, wedge-shaped piece of the lung that contains the tumour, along with a thin border of healthy tissue to be safe.
This is usually the best option for very small, early-stage tumours found on the outer edges of the lung. It’s also ideal for patients whose overall lung function might not be strong enough for a larger operation. Think of it as carefully trimming a single leaf or a tiny twig, leaving the main branch completely intact.
Segmentectomy: Removing a Full Lung Segment
A segmentectomy goes one step further. Instead of just a small piece of tissue, this operation removes an entire segment of a lobe—a complete, self-contained unit with its own airway and blood vessels. This is like removing a whole smaller branch from one of the main limbs of the tree.
This approach is becoming a fantastic option for small, early-stage cancers. It finds a crucial balance between making absolutely sure all the cancer is gone while preserving as much healthy, functioning lung as possible. By saving the rest of the lobe, a segmentectomy generally has less impact on your breathing capacity once you’ve recovered.
Lobectomy: The Gold Standard for Lung Cancer
The lobectomy is the most common surgery for lung cancer and is widely considered the gold standard for treating early-stage disease. This operation involves removing an entire lobe of the lung—one of those main limbs from our tree analogy.
Taking out the whole lobe gives us the best chance of removing not just the tumour, but also any nearby lymph nodes where cancer cells might have lodged. While it's a bigger operation than a wedge or segmentectomy, people are often surprised at how well they adapt. The remaining lobes actually expand over time, helping to make up for the part that was removed.
"I remember asking Mr Scarci, ‘Will I be able to breathe properly after you take out a whole lobe?’ He was very reassuring. He explained that my other lobes would work a bit harder and that physiotherapy would be key. He was right. It took time, but I got back to my daily walks, and that was a huge milestone for me." – John, Lobectomy Patient
Pneumonectomy: Removing an Entire Lung
A pneumonectomy is the most extensive lung operation we perform, as it involves removing an entire lung. This is only ever done when it's absolutely necessary—for instance, when a tumour is very large and centrally located, tangled up in the main airways or blood vessels. In our tree analogy, this is like taking out the whole tree on one side.
This is a major operation, and it's only a suitable option for patients who have excellent function in their other lung. Before even considering a pneumonectomy, we run exhaustive tests to make certain you can live a full and active life with just one lung. It’s a decision we weigh with immense care, always balancing the need to cure the cancer with your long-term quality of life.
A Closer Look at Minimally Invasive Surgery Options

The very idea of surgery can be daunting, often conjuring images of large scars and long, difficult recoveries. Thankfully, that picture is becoming a thing of the past. Surgical techniques have moved on significantly, and today, most lung cancer surgery is performed using minimally invasive methods.
These modern approaches, often called "keyhole surgery," accomplish the exact same goals as traditional open surgery but without the need to spread the ribs. This single change makes an enormous difference to your experience, leading to less pain, a shorter hospital stay, and a much quicker return to your normal life. Let’s look at the two leading techniques I specialise in.
Video-Assisted Thoracoscopic Surgery (VATS)
Video-Assisted Thoracoscopic Surgery, or VATS, is the most common and well-established type of keyhole lung surgery. Instead of making one long incision, I make a few small cuts, usually only between 1 and 5 centimetres long.
Through one of these small openings, I insert a tiny high-definition camera known as a thoracoscope. This provides a crystal-clear, magnified view of the inside of your chest on a monitor in the operating theatre. I then use specially designed, long-handled instruments through the other incisions to carefully perform the operation, whether it's a wedge resection, a segmentectomy, or a lobectomy.
The real game-changer with VATS is that we avoid spreading the ribs apart. This dramatically reduces the pain you feel after the operation and helps you get back on your feet much, much faster.
Robotic-Assisted Surgery
Robotic-assisted surgery builds on the principles of VATS but adds another layer of technological refinement. I work from a dedicated console within the operating theatre, controlling a set of highly sophisticated robotic arms which hold the camera and surgical tools.
This system gives me an incredibly detailed, 3D high-magnification view. More than that, the robotic instruments have tiny "wrists" that can bend and rotate far beyond the capability of the human hand. This allows for exceptionally precise and steady movements, which can be invaluable for more complex procedures or when dealing with tumours in particularly tricky-to-reach spots.
"I was worried about being off my feet for a long time, but Mr Scarci explained the keyhole approach. The recovery was so much faster than I expected. I was home in a few days and walking around my garden within a week. It made all the difference to my mindset and my physical healing." – A Patient's Experience
The shift towards these advanced procedures is clear. In England recently, a record 7,018 lung resections with curative intent were performed for non-small cell lung cancer, up from 5,865 the year before. While this shows a brilliant trend in getting patients the surgery they need, it also highlights the growing pressure on NHS services. You can see more data in the 2025 National Lung Cancer Audit report.
Comparing the Benefits
To help you understand the differences, here’s a quick comparison of the three main surgical approaches.
Comparing Open, VATS, and Robotic Lung Surgery
| Feature | Open Surgery (Thoracotomy) | VATS Surgery | Robotic Surgery |
|---|---|---|---|
| Incision Size | One long incision (15-20 cm) | 2-4 small incisions (1-5 cm) | 3-5 very small incisions (<2 cm) |
| Rib Spreading | Yes, ribs are spread apart | No rib spreading | No rib spreading |
| Post-Op Pain | Significant | Minimal to moderate | Minimal |
| Hospital Stay | Typically 5-7 days or more | Typically 2-4 days | Typically 1-3 days |
| Recovery Time | Several months | A few weeks | A few weeks |
| Surgeon's View | Direct vision | 2D magnified view on a monitor | 3D high-definition, magnified view |
| Instrumentation | Standard surgical instruments | Long, straight instruments | Articulated "wristed" instruments |
As you can see, both VATS and robotic surgery offer huge advantages over a traditional open thoracotomy. The best approach for you will always depend on the specifics of your case, but the shared benefits of keyhole surgery are compelling.
Key Advantages of Minimally Invasive Techniques:
- Less Post-Operative Pain: By avoiding a large cut and rib spreading, you'll experience far less discomfort.
- Shorter Hospital Stay: Most people are able to go home within 2-4 days, a big difference from a week or more with open surgery.
- Faster Recovery Time: You can get back to daily activities, like driving and light work, in just a few weeks.
- Reduced Scarring: The small incisions are much less noticeable once healed.
- Lower Risk of Complications: There's generally a lower risk of issues like infection and bleeding.
It is important to know that while keyhole surgery is my preferred method, there are times when a planned open operation is the safest choice for a patient. Very rarely, a keyhole procedure might need to be converted to an open one during surgery. I've written more about the reasons for a VATS conversion to open surgery in this detailed guide. This decision is never taken lightly and is always made with your safety as the number one priority.
Your Step-by-Step Guide to Lung Cancer Surgery
Facing lung cancer surgery can feel overwhelming, but understanding the path ahead can make a world of difference. Knowing what to expect, from your first appointment right through to your recovery at home, helps take the fear of the unknown out of the equation. It allows you to focus your energy on healing.
Here’s a look at the typical journey, whether you’re coming through the NHS or a private, fast-track pathway.
This diagram gives you a bird's-eye view of the entire process, from the initial tests to getting you back on your feet.
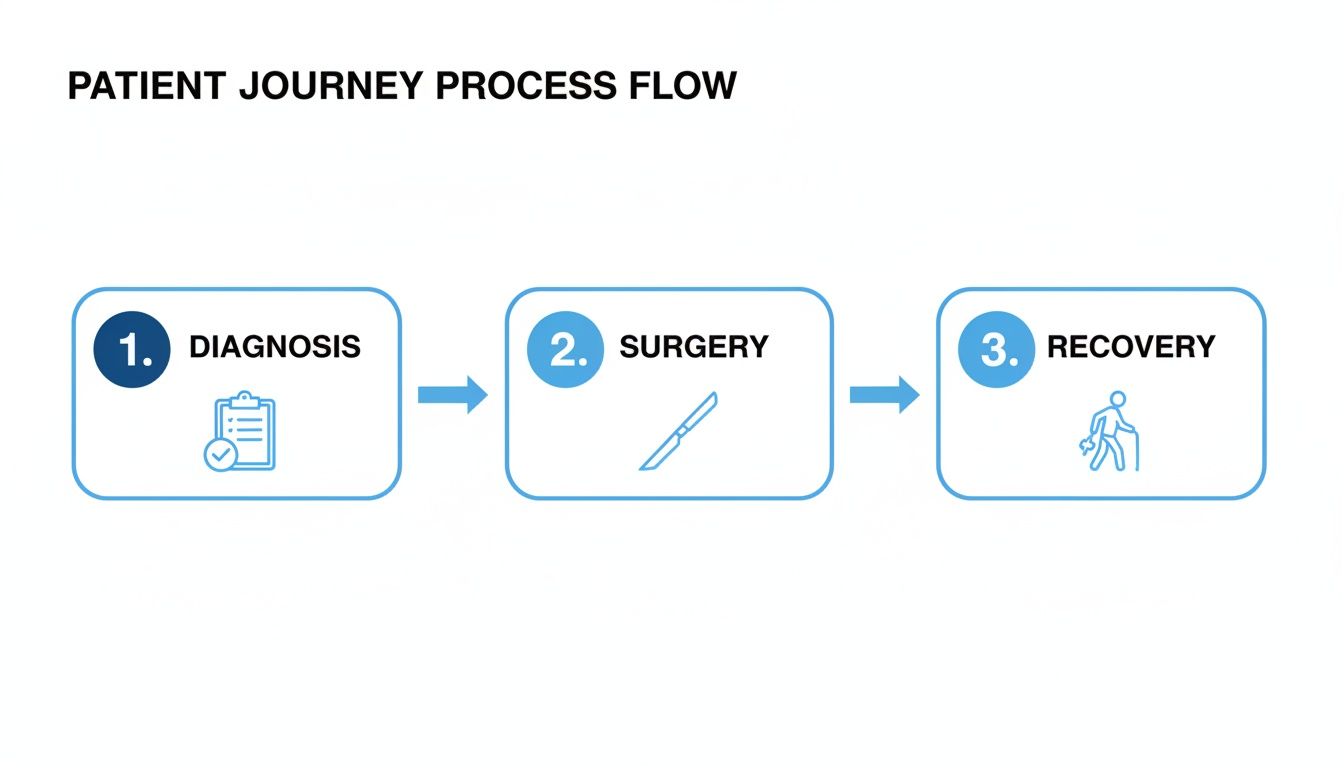
As you can see, it's a structured journey. We move methodically from assessment to the operation itself, and finally into a dedicated period of post-operative care and recovery.
Getting You Ready for Surgery: The Pre-Op Assessment
After the multidisciplinary team (MDT) has reviewed your case and confirmed that surgery is the best course of action, the first step is a thorough pre-operative assessment. Think of this as a complete 'MOT' for your body. It's not just a box-ticking exercise; it's a vital safety check to ensure you're in the best possible shape for the procedure.
We’ll run a few key tests to get a complete picture of your health:
- Lung Function Tests (Spirometry): A simple but powerful breathing test that shows us how much air your lungs hold and how efficiently you can move it. This helps us predict how well you’ll breathe with the remaining lung tissue after surgery.
- Cardiopulmonary Exercise Test (CPET): This involves you cycling on a stationary bike while we monitor your heart and lung response. It’s the gold standard for measuring your overall fitness for surgery.
- Imaging Scans: We’ll often take a final CT or PET-CT scan. This gives us an up-to-the-minute, high-definition map of the tumour’s location and size, which is critical for precise surgical planning.
- Blood Tests: These standard tests give us a baseline of your general health, checking everything from kidney function to your blood count.
The emotional weight of a cancer diagnosis and major surgery can also be immense. For many, exploring the healing power of counselling for depression can be an incredibly helpful part of the healing process.
Timelines: NHS vs. Private Pathways
How long will you have to wait? The timeline from diagnosis to surgery can vary. In the NHS, the national target is to treat patients within 62 days of an urgent GP referral. While everyone works incredibly hard to hit this goal, system pressures can sometimes cause delays.
In my private practice, we can often significantly reduce that waiting period. My aim is to see you for an initial consultation within a couple of days of a referral. From there, we can frequently schedule surgery within one to two weeks. Moving quickly like this doesn't just treat the cancer sooner; it dramatically cuts down on that stressful, anxious waiting time.
Your Hospital Stay and First Steps to Recovery
On the morning of your surgery, you’ll meet with both the anaesthetist and me. We’ll run through the plan one last time and answer any final questions you might have. The operation itself, whether it’s a VATS or robotic procedure, is done while you're asleep under a general anaesthetic.
Afterwards, you’ll spend a short time in a recovery area before being moved to the ward. In these first few hours and days, our focus is squarely on three things: keeping you comfortable with effective pain management, helping you get up and moving, and guiding you through breathing exercises to help your lung re-expand fully.
A question I get asked all the time is, ‘Am I too old for this operation?’ It’s a completely understandable concern. But what we’ve learned over the years is that fitness trumps age, every time.
Recent UK screening studies have shown that older patients who are fit enough for surgery get just as much survival benefit as younger patients. Data shows that the four-year mortality rate for the 75-80 age group was almost identical to that of younger patients (16% vs 18%). This is powerful evidence that age alone shouldn't stop anyone from getting curative treatment. You can read more about these important lung cancer screening findings.
Thanks to modern, minimally invasive techniques, your hospital stay is likely to be quite short – typically just two to four days. Once we’re happy you’re safe to go home, we’ll discharge you with a personalised recovery plan. To understand more about what to expect during this phase, you can read our detailed guide on the journey of post-surgery recovery for lung cancer.
Why Choose a Specialist Thoracic Surgeon?
When you’re facing something as significant as lung cancer surgery, perhaps the most critical decision you'll make is who you trust to perform it. This isn't simply about finding a qualified doctor; it’s about finding a true specialist whose entire career is dedicated to your specific problem. A thoracic surgeon focuses exclusively on the chest, which means they live and breathe complex lung operations day in, day out.
That level of focus really matters. Surgeons who perform a high volume of procedures like VATS and robotic lobectomies develop an almost intuitive skill and precision. This experience directly translates into better outcomes for you, a smoother recovery, and the confidence of knowing they are prepared for any complexities that might come up during surgery.
It’s Not Just About the Surgery
Beyond the operating theatre, the right surgeon understands that you are a person, not just a set of scans. A patient-centred approach is about building a relationship based on clear communication, empathy, and genuine support for you and your family.
My entire practice is built around this philosophy. From our very first conversation, my team and I make it our mission to understand your personal concerns and what matters most to you. We take the time to answer every single question, no matter how small, so you feel confident and in control of your journey. This partnership is fundamental to navigating the path ahead.
"I needed someone who saw me, not just my scans. Mr Scarci explained everything in a way I could understand. That trust made all the difference in the world. I knew I was in the safest possible hands." – A Former Patient
A Clear and Rapid Path to Treatment
We know that waiting is one of the hardest parts. That’s why we’ve designed a straightforward, rapid-access pathway, whether you have private medical insurance with providers like Bupa, AXA, or Aviva, or are funding the treatment yourself. Our goal is to get you from that initial consultation to treatment in about a week, cutting down on unnecessary anxiety.
Getting started is simple. You can ask your GP or consultant for a direct referral to my practice. Once we receive it, my team will be in touch to arrange an appointment, usually within 24-48 hours. We provide complete clarity on any costs involved and are happy to help you manage the insurance authorisation process.
Making this first decision is a huge step, and our guide on how to choose a lung cancer surgeon in London can offer more help. By choosing an expert team, you're not just getting an operation; you're getting comprehensive care designed to give you the best possible result.
Frequently Asked Questions
It’s completely normal to have a long list of questions when you're thinking about lung cancer surgery. I’ve put together some straightforward answers to the concerns I hear most often from my patients, hoping to give you a clearer picture of what to expect.
How Long Does Recovery Take After Lung Cancer Surgery?
Recovery is different for everyone and depends on the specific operation and your fitness levels, but it’s much quicker than it used to be. With modern minimally invasive surgery (VATS or robotic), most of my patients are home from the hospital in just two to four days.
You'll likely start feeling more like your old self within four to six weeks. But remember, it’s a gradual journey, and a full recovery can take a few months. We'll give you a tailored plan to manage any discomfort, get you started on crucial breathing exercises, and help you ease back into activity at your own pace.
Will My Breathing Feel Normal After Surgery?
This is a very common and understandable worry. Before any surgery is planned, we carry out detailed lung function tests to make absolutely sure you can comfortably tolerate the operation we have in mind. You might notice some breathlessness at first, but your remaining lung tissue is remarkable and will gradually adapt and expand to compensate.
The vast majority of patients adjust extremely well and get back to their daily routines without any significant breathing problems. Following a structured physiotherapy programme after your operation is key to getting the very best out of your lung capacity.
"I was convinced I wouldn't be able to walk up the stairs without getting breathless. For the first week, it was tough. But I did the exercises Mr Scarci’s team gave me, and every day got a little easier. Three months later, I was back on my daily dog walk, and it felt like a huge victory." – A Patient's Reflection
What Are the Main Risks of This Surgery?
Every operation has potential risks, and my team and I take every possible precaution to keep them to an absolute minimum. The more common issues we watch out for are things like infection, bleeding, a persistent air leak from the lung, or a reaction to the anaesthetic.
Less common, but more serious, complications can include things like pneumonia or blood clots. When we meet, we will talk through all of these potential risks as they specifically apply to you and your health, so you have all the information you need to make a confident decision about your care.
Will I Need More Treatment After My Operation?
Whether or not you need further treatment—what we call adjuvant therapy—depends entirely on what the final pathology report tells us about the tissue we removed.
If the detailed analysis shows that cancer cells have reached the lymph nodes, or if the cancer is at a more advanced stage than we first thought, we might recommend chemotherapy or radiotherapy. The goal here is to give you the best possible chance of the cancer not returning. This is never a decision made in isolation; your case will be discussed in detail by our full multidisciplinary team (MDT) of specialists.
If you have other questions on your mind or would like to talk about your own situation, please don’t hesitate to get in touch with my team. At Marco Scarci Thoracic Surgery, our focus is on providing swift, expert care that gives you confidence and clarity. You can arrange a consultation directly through our website: https://marcoscarci.co.uk.