For anyone with pectus excavatum, surgery in the UK can offer a permanent fix for a sunken or 'funnel' chest. The good news is that treatment is available through both the NHS and private healthcare. Your options will typically boil down to either the minimally invasive Nuss procedure or the more traditional Ravitch technique, with the final choice depending on your specific anatomy and clinical needs.
Your Starting Point for Pectus Excavatum Surgery
Living with pectus excavatum can be tough. It often starts in the teenage years and can affect everything from your breathing and comfort to your self-confidence. For many, it's a very private struggle. But the first real step towards taking back control is understanding exactly what's going on.
Think of your chest wall as a flexible frame. With pectus excavatum, the cartilage that links your ribs to the breastbone (the sternum) grows in an unusual way. This growth pattern pulls the sternum inwards, creating that characteristic dip or indentation. It's actually the most common congenital chest wall deformity out there, not just in the UK but worldwide. However, the path to getting treatment, particularly pectus excavatum surgery in the UK, has its own specific system to navigate.
Understanding Your Surgical and Non-Surgical Options
When you start looking at treatments, it helps to visualise how you might reshape that chest framework. The two main surgical methods tackle this in quite different ways.
- The Nuss Procedure: This is the minimally invasive route. A surgeon inserts a curved metal bar behind your sternum, which then acts as an internal brace to push the chest forward into the right position. After about 2-3 years, once the cartilage has set in its new shape, the bar is removed.
- The Ravitch Procedure: This is a more traditional, open surgery. It involves the surgeon directly removing the abnormal cartilage and physically repositioning the sternum. This approach is often better suited for more complex cases or for older patients whose chests are not as flexible.
Pectus excavatum is just one of several common chest wall deformities that specialist surgeons can treat.
While surgery provides a permanent solution, it's also useful to know about non-surgical alternatives. The Vacuum Bell, for example, is a device that creates suction to gradually lift the sternum over a long period. It takes dedication and works best on younger patients with more pliable chests, but for some, it can be a less invasive first step.
The condition is more widespread than you might think, affecting roughly 1 in 400 births in the UK and being about five times more common in males. Because of the physical and psychological toll it can take, NHS England carries out around 380 corrective surgeries each year for severe cases. This official recognition highlights the huge difference surgery can make to both physical function and overall quality of life.
The goal of this guide is to demystify the medical terms and build a solid foundation of knowledge. Armed with this understanding, you can confidently explore the NHS and private pathways available for pectus excavatum surgery in the UK.
Getting Pectus Surgery on the NHS: What's Involved?
If you're looking to have pectus excavatum surgery through the NHS in the UK, it’s a journey with some very specific steps. The first thing to understand is that funding has become much tighter over the last few years; it’s now reserved for people with the most severe, physically impactful cases.
Everything kicks off with a visit to your GP. This is your starting line.
Your First Step: The GP Consultation
When you see your doctor, it's vital to be clear about everything you're experiencing. Don't just talk about how your chest looks—focus on the physical symptoms. Are you getting breathless? Can you not keep up with friends when exercising? Do you ever get chest pain? These details are crucial.
If your GP believes your case needs a specialist's eye, they will refer you to a thoracic surgeon. This won't be at your local hospital, but at one of the few specialist NHS centres that handle this type of surgery.
Meeting the Strict NHS Criteria
Once that referral comes through, you'll go through a series of in-depth tests to see if you qualify for surgery on the NHS. The key metric they use is something called the Haller Index. It’s a number calculated from a CT scan that gives a precise measurement of how deep the dip in your chest is.
To even be considered for NHS-funded surgery, your Haller Index score typically needs to be 3.25 or higher. But that’s not all. You must also have clear clinical proof that the shape of your chest is physically squashing your heart or lungs and affecting how they work.
The days of getting this surgery on the NHS for purely cosmetic or psychological reasons are gone. The focus now is squarely on fixing a significant physiological problem.
The flowchart below gives you a good idea of the different routes you might take after being diagnosed with pectus excavatum.
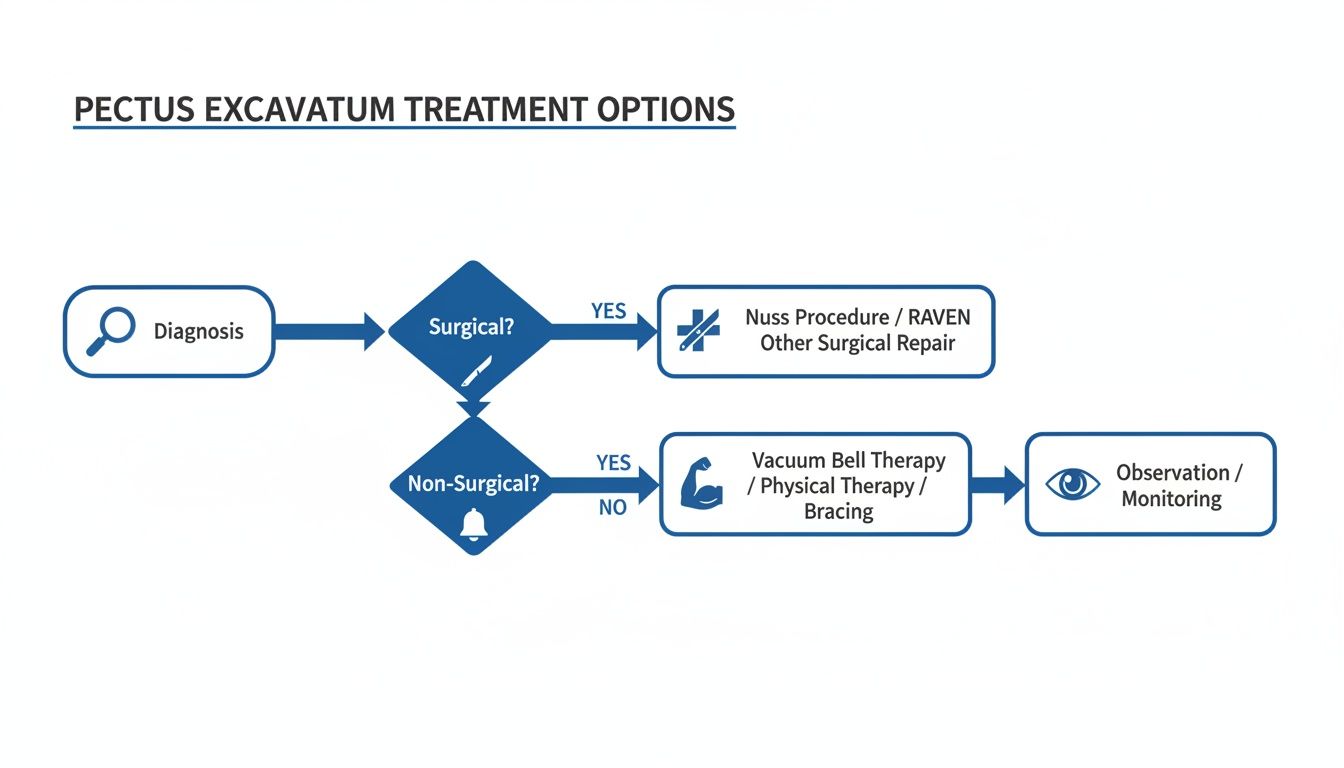
As you can see, once a diagnosis is made, the path splits depending on whether surgery is the right choice, which then leads to more evaluations and specific procedures.
The National Review Panel and the Long Wait
Even if you meet the initial criteria, your case isn't approved just yet. It gets passed to a national Multi-Disciplinary Team (MDT). This is a panel of experts who will pore over all your results—your scans, your heart and lung function tests—to make the final call on funding.
If you get the green light, you’re then added to the surgical waiting list.
It's so important to be realistic about how long all of this takes. The NHS pathway can mean a long wait for your first specialist appointment, another wait for all the tests, and then an even longer one for the surgery itself. Thinking through all your options from the start is wise, which is why navigating both NHS and private healthcare options can be a really helpful exercise.
The situation has changed a lot recently. Back in 2019, NHS England paused routine funding for this operation. Thankfully, this was reviewed, and in 2023, funding was brought back for severe cases, but only when assessed by the national MDT and performed at just two specialist hospitals in the UK. For a deeper dive into how the two systems stack up, you can check out our guide on the NHS vs private sectors.
Adding to this, a major clinical trial called RESTORE, funded by the NIHR, kicked off in 2024. Its goal is to properly compare surgical results against non-surgical treatments, which will no doubt shape how pectus excavatum is treated in the years to come.
Exploring the Private Route for Pectus Surgery
For many people in the UK, the strict NHS criteria and long waiting lists can feel like an impossible barrier. If you're looking for a more direct path to treatment, going private for pectus excavatum surgery in the UK is a realistic alternative that puts you back in the driver's seat.
Going private is all about control. You get to choose your surgeon and the hospital where you feel most comfortable. Most importantly, it completely changes the timeline. What can often take years on the NHS can be condensed into a matter of weeks, moving you from initial consultation to surgery with incredible speed.

Understanding the Costs of Private Surgery
Naturally, one of the first questions on anyone's mind is, "What's this going to cost?" Good private clinics are completely transparent about this, typically offering a single package price that covers every step of the journey.
A standard self-pay package for pectus excavatum surgery in the UK will almost always cover:
- Initial Consultation: Your first in-depth meeting with the surgeon.
- Diagnostic Imaging: All the essential scans, like CTs, needed to map out the procedure.
- Surgeon and Anaesthetist Fees: The cost for your expert medical team.
- Hospital Fees: This bundles in the operating theatre, your room, nursing care, and medications.
- Follow-up Appointments: Crucial post-op check-ups to make sure you're healing well.
The final figure can shift based on the hospital, your surgeon's fees, and how complex your specific case is. It’s absolutely vital to get a detailed, all-inclusive quote from your clinic so there are no hidden surprises down the line.
Opting for private treatment means you are paying for speed, choice, and a streamlined care pathway. The focus is on getting you from diagnosis to recovery as efficiently as possible, with a team you have selected yourself.
How to Fund Your Private Pectus Surgery
Once you have a clear cost, the next hurdle is figuring out how to pay for it. There are really two main ways people fund their surgery in the private sector.
Self-Funding: This is the most direct route, where you pay for the treatment yourself. Many clinics understand this is a significant outlay and offer payment plans or work with specialist medical finance providers to help you spread the cost. It’s well worth exploring the different finance options for thoracic surgery in the UK to see what might fit your budget.
Private Medical Insurance: If you already have a private health insurance policy, it might well cover pectus excavatum surgery. But this is a big "if". Policies and providers vary wildly. You must call your insurer at the very beginning of the process to confirm exactly what is and isn't covered. Get their pre-authorisation before you book a single consultation.
A Patient's Story: My Journey Through Surgery and Recovery
You can read all the medical facts and figures in the world, but nothing quite explains the journey of pectus excavatum surgery like hearing from someone who’s actually been through it. This is Liam’s story. A 26-year-old graphic designer from Birmingham, he decided to take action after years of feeling held back by his condition.
"I’d been aware of my 'dent,' as I used to call it, since I was a teenager," Liam begins. "It was more than just being a bit self-conscious. I was that kid who always kept his T-shirt on at the swimming pool, the one who’d make excuses to get out of beach trips with mates. But it was the physical side of it that really started to grind me down in my twenties."
Liam’s experience echoes what many people with pectus excavatum go through. He describes a constant, dull pressure in his chest, getting out of breath way too easily, and the unnerving feeling of his heart racing after something as simple as climbing a few flights of stairs.
Making the Decision to Act
The final push for Liam came after a frustrating five-a-side football match. "I was absolutely gasping for air after just a few minutes of running," he remembers. "My friends were worried, and I was just embarrassed. I realised right then that this wasn't just about how I looked; it was actively getting in the way of my life. That night, I went home and started seriously searching for pectus excavatum surgery UK."
His GP referred him to an NHS specialist, but the long waiting list and strict criteria led him to look into private options. He booked a consultation, had his scans done within a week, and was given a surgery date just a month later.
"The speed of it all was incredible," Liam says. "Suddenly, something that had always felt like a distant possibility was real and happening very soon. Of course, that brought a huge wave of anxiety. The night before the op was completely sleepless, just a blur of 'what ifs.' But I have to say, the surgical team was fantastic at putting my mind at rest."
The Surgery and Hospital Stay
Liam had a minimally invasive Nuss procedure. When he woke up, he felt groggy and pretty sore, but the very first thing he noticed was the shape of his chest. "Even with all the bandages on, I could see it was different. It was flat. For the first time in my life, it just looked… normal. That feeling was immense."
He spent five days in the hospital. The first couple were the toughest, with the focus squarely on managing pain and doing gentle breathing exercises. The nurses showed him how to move carefully—learning to log-roll out of bed became an essential skill to avoid putting any strain on his chest muscles.
"The first deep breath I took without that old, familiar restriction was a total revelation. It honestly felt like my lungs suddenly had more space, more freedom. It was a small victory, but it meant absolutely everything."
It's easy to forget the psychological weight of pectus excavatum. Studies have shown that a high number of patients report feelings of anxiety (65%) and depression (65%), with 80% feeling bothered by the appearance of their chest. Liam's story really brings these numbers to life, showing the profound emotional relief that correcting the condition can bring.
Navigating Recovery at Home
The first few weeks back home were a real test of patience. Liam had a strict set of rules to follow: no lifting anything heavier than a carton of milk, no twisting his body, and no raising his arms above his head. He also had to sleep on his back, propped up by a mountain of pillows.
"It was a challenge, for sure," he admits. "You just don't realise how much you use your core and chest for everyday things until you can't. But every single day was a tiny bit better than the one before. I started celebrating the small milestones—walking a little further down the road, being able to sit up on my own, and finally, the day the surgical dressings came off."
Six weeks after his operation, Liam was given the green light to go back to his desk job and start some light activities. The change in him was remarkable.
"My energy levels were just through the roof," he says, smiling. "The breathlessness was gone. The heart palpitations had completely stopped. It was like a weight I'd been carrying around my entire life had finally been lifted."
Three years on, Liam had the bar removed in a straightforward day-case procedure. Today, he lives a life free from the physical and mental burden of pectus excavatum. "Looking back, going through with the surgery was the best decision I ever made," he reflects. "My advice to anyone thinking about it is to do your research, speak to the specialists, and don't underestimate the positive change it can make in your life. It’s not just about changing your chest; it's about reclaiming your confidence and your freedom."
Preparing for Surgery and Mastering Your Recovery
Going through with pectus excavatum surgery is a big decision, and honestly, the work you put in before and after is just as crucial as the operation itself. It helps to think of it as a project. You have a clear goal, distinct phases, and milestones to hit. This mindset puts you in the driver's seat and sets you up for a much smoother, more confident healing journey.
Success really does start weeks before you even see the operating theatre. Your surgical team will give you a detailed plan, but the main idea is simple: get your body into the best possible shape to handle the stress of surgery and bounce back faster.

Your Realistic Recovery Timeline
Recovery doesn’t happen all at once; it unfolds in stages. Knowing what’s coming can take a lot of the anxiety out of the process and helps you appreciate the small wins along the way.
In the Hospital (Typically 3-7 Days)
- Pain Management is Key: Let's be frank, the first 48-72 hours are the toughest. Your team will have a carefully managed pain relief plan, often using an epidural or a system you control yourself (PCA).
- Getting Moving: The nurses will help you get out of bed and into a chair surprisingly quickly, sometimes the day after surgery. It might feel like the last thing you want to do, but it’s vital for preventing complications like blood clots.
- Breathe Deep: You’ll keep up with those breathing exercises you practised at home. This is essential for keeping your lungs clear and warding off infections.
At Home (Weeks 1-6)
- Rest and Rules: The first few weeks are all about letting your body heal. You’ll have strict instructions: no lifting, no twisting, no pushing. You'll need to master sleeping on your back, probably propped up with a fortress of pillows.
- Wound Care: You'll get clear guidance on looking after your incisions. Following this helps them heal cleanly and minimises scarring down the line.
- Managing Expectations: You are going to feel exhausted. That is completely normal. Listen to your body and resist the urge to do too much too soon. The mental game is just as important—stay positive and focus on the small, day-to-day improvements.
Your surgical team is your lifeline during this period. Never, ever hesitate to call them if you have a question about pain, your wounds, or anything else that’s worrying you. Good communication is the bedrock of a safe recovery.
As you start feeling better, you'll naturally wonder what you can and can't do. It's helpful to start understanding your functional capacity, which is a way of objectively measuring your physical abilities. This can be incredibly empowering as you get ready to ease back into more demanding activities.
It’s reassuring to know that between 300 and 380 pectus excavatum correction surgeries are performed each year in the UK, which shows just how established these procedures are. The less invasive Nuss procedure is now the most common choice, and clinical audits consistently show very low mortality rates (<1%) and manageable complication rates for things like bar displacement or infection. These excellent safety records are backed by NHS commissioning policies aimed at getting the best possible results for every patient.
Your Pectus Surgery Questions Answered
When you're considering surgery for pectus excavatum, a hundred questions are probably running through your mind. That’s completely normal. Here, we’ll tackle some of the most common queries we hear from patients, breaking down the answers in a straightforward way.
How Long Does Recovery Really Take After Pectus Surgery?
Recovery is a journey, not a sprint, and it looks a bit different for everyone. Straight after the operation, you can expect to be in the hospital for about 3 to 7 days. The main focus during this time is getting pain under control and gently getting you back on your feet.
The first 4 to 6 weeks back at home are all about protecting your chest as it heals. This means no heavy lifting, twisting, or pushing. Many people can get back to a desk job or their studies during this window, but you’ll need to be mindful of your movements.
After about 6-8 weeks, you'll likely be cleared for light exercise like walking. But for anything more intense – think contact sports or heavy gym sessions – you’ll need to wait at least 3 months. Your surgical team will give you a detailed, personalised timeline so you know exactly what to expect.
Is the Bar from the Nuss Procedure Permanent?
No, it isn't. Think of the metal bar used in the Nuss procedure as internal scaffolding. Its job is to hold your breastbone in its new, corrected position while your body adapts.
This bar typically stays in place for 2 to 3 years. That’s how long it takes for the cartilage in your chest to remodel and permanently set in its new shape. After that time, the bar is taken out during a second, much more straightforward day-case procedure, and the recovery is far quicker than the first time around.
What Are the Main Risks of the Surgery?
Every major operation comes with risks, and it’s vital to talk these through with your surgeon. Thankfully, with an experienced team, serious complications are rare.
- Pain After Surgery: This is the most common challenge, but it's something we plan for. It’s managed with a comprehensive pain relief plan, often starting with an epidural while you're in the hospital.
- Pneumothorax (Collapsed Lung): This can happen, but it is almost always spotted and dealt with by the surgical team right away.
- Infection or Bleeding: As with any surgery, there's a small risk of infection around the incision sites or some internal bleeding.
- Bar Displacement (Nuss Procedure): In a small number of cases, the bar can shift. If this happens, it usually just requires a minor procedure to put it back in the right place.
Your surgeon will go over all the potential risks as they apply to your specific health and circumstances, making sure you have all the information you need.
Understanding the potential risks is a crucial part of the consent process. A good surgical team will be transparent and answer every question you have, ensuring you feel confident and prepared.
Can I Get Surgery for Cosmetic Reasons on the NHS?
This is a really common question. Under the current NHS England policy, surgery isn't funded if the reasons are purely cosmetic.
To qualify for NHS-funded pectus excavatum surgery in the UK, you need to meet strict clinical criteria. This typically means having a severe deformity (usually a Haller Index over 3.25) combined with clear medical evidence that the condition is physically affecting you—for instance, by compressing your heart or lungs and interfering with their function.
If you don't meet these criteria but are still struggling with the psychological impact or appearance of your chest, you would need to look at private healthcare options.
At Marco Scarci Thoracic Surgery, we know that deciding on surgery is a major step. Mr Scarci provides rapid access to consultations, offering clear, expert guidance to help you navigate your options and find the best path for your health and wellbeing. To find out more or to book an appointment, please visit the Marco Scarci official website.