In this comprehensive guide, I will provide information on what a pleural biopsy and a pleurodesis procedure are, what doctors use them for, how they are performed, and what to expect.
In patients with malignant pleural effusion, these procedures have helped countless individuals.
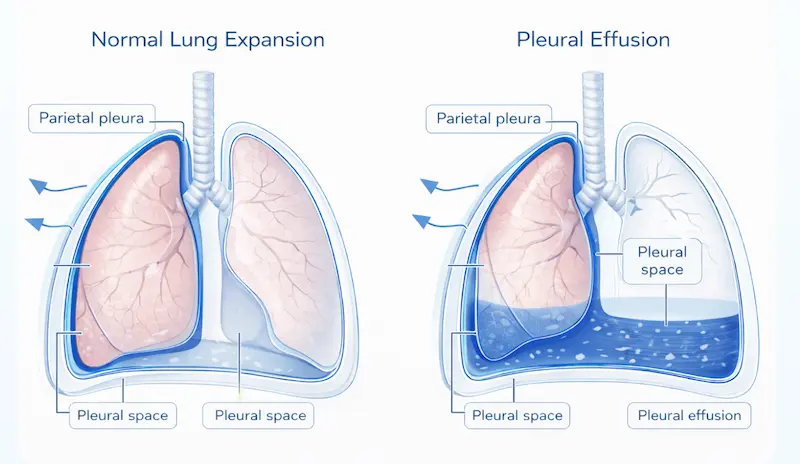
Your lungs are remarkable organs, protected by a delicate, thin membrane called the pleura. Think of the pleura as a gentle, protective layer around your lungs and chest wall – two smooth layers (parietal pleura and visceral pleura) that allow your lungs to expand and contract effortlessly with each breath. When something affects this area, it can impact your breathing, comfort, and overall well-being.
Sometimes, pleural fluid accumulates in the space between the lung and the chest wall, known as the pleural cavity. You can think of it as a box where, usually, a balloon full of air (the lung) touches the inside of the box. If you pour water into the box, the balloon shrinks and doesn’t inflate as well.
When your doctor recommends a pleural biopsy, they’re essentially saying:
“We want to gather the most accurate information possible so we can provide you with the best care.”
A doctor’s recommendation for a pleural biopsy is not a sign that something terrible is happening—it shows that your medical team is being thorough, careful, and committed to getting you the proper treatment.
Sometimes fluid accumulates around the lungs, causing discomfort, breathlessness, or chest pain. A biopsy helps identify exactly what’s causing this fluid buildup, whether it’s an infection that responds to antibiotics (parapneumonic effusion), inflammation that responds to specific medications (recurrent pleural effusion), or another condition that requires targeted therapy. Sometimes fluid accumulation is caused by cancer, which we call malignant effusion.
For individuals with potential asbestos exposure, a biopsy can provide crucial diagnostic information on conditions such as mesothelioma. Specialist teams who diagnose mesothelioma understand the unique concerns of patients with occupational exposures and provide both medical care and emotional support throughout the diagnostic process.
Sometimes, what appears concerning on imaging studies turns out to be a treatable infection, such as tuberculosis. A biopsy can quickly identify these conditions, leading to targeted antibiotic treatment and complete recovery.
If there’s any concern about cancer, a biopsy provides definitive answers. While the word “cancer” naturally causes fear, remember that early detection and accurate staging are your greatest allies. Many lung cancers respond well to treatment when caught early. Malignant pleural mesothelioma, an incurable cancer of the lining of the chest wall, can also cause fluid buildup.
This is often the first approach considered.
Using advanced imaging guidance, such as ultrasound or CT scans, your doctor guides a thin needle to the precise location.
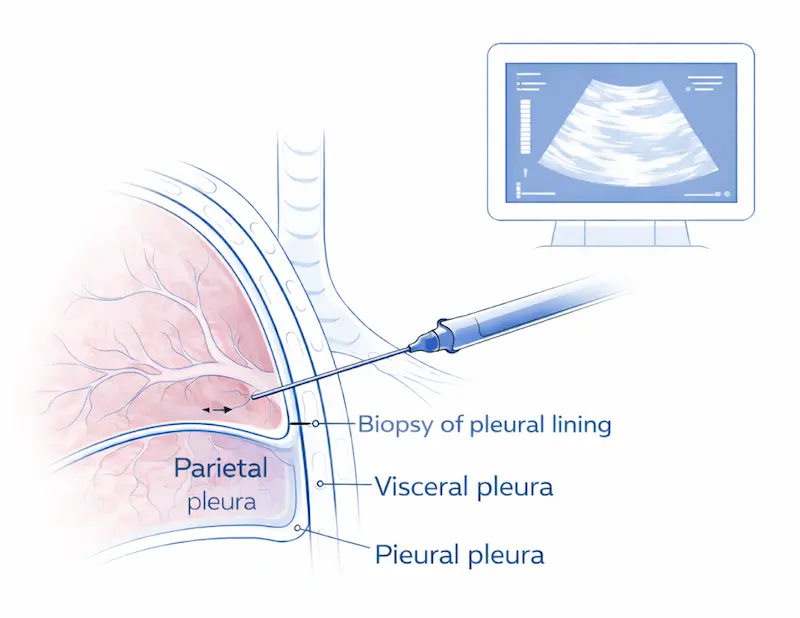
This represents the gold standard in minimally invasive chest surgery. Doctors often consider this technique the standard approach when larger tissue samples are needed, while still maintaining the benefits of minimal invasiveness – smaller incisions, less pain, and faster recovery. The diagnostic yield of this procedure is much higher than that of any other technique in diagnosing any pleural abnormality.
Before considering surgery, your medical team may explore other treatment options:
The procedure typically takes 30-90 minutes, depending on the approach used. You’ll receive appropriate anaesthesia – either local anaesthesia for needle biopsies or sedation for thoracoscopic procedures. Expert anaesthesia services ensure you’re comfortable throughout the entire process.
Immediately after your procedure, nursing staff will carefully monitor you in a recovery area, check your vital signs, and ensure you’re feeling well.
Comprehensive post-procedure care includes pain management, home care instructions, and scheduling follow-up appointments.
Our team guides you through every step of the biopsy process.
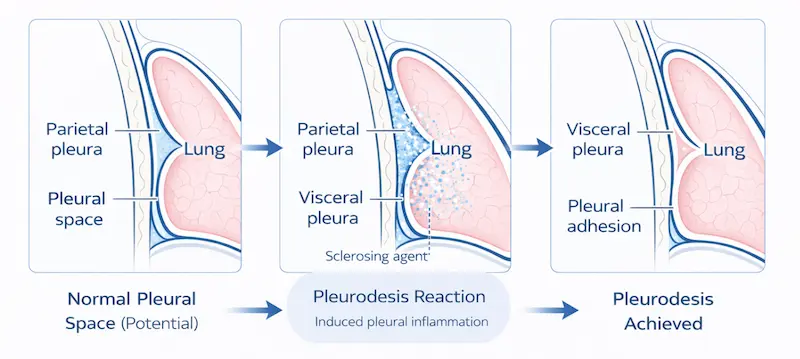
Pleurodesis works by inducing a controlled, therapeutic inflammatory response that causes the two pleural layers to adhere.
While the word “inflammatory” might sound concerning, it actually describes a carefully orchestrated healing process that eliminates the space where fluid or air can accumulate.
imagine having a space between two surfaces where water keeps collecting. Pleurodesis eliminates that space by bringing the surfaces together, preventing future water accumulation.
Personalised pleurodesis treatment plans take into account your specific condition, overall health, previous treatments, and personal preferences.
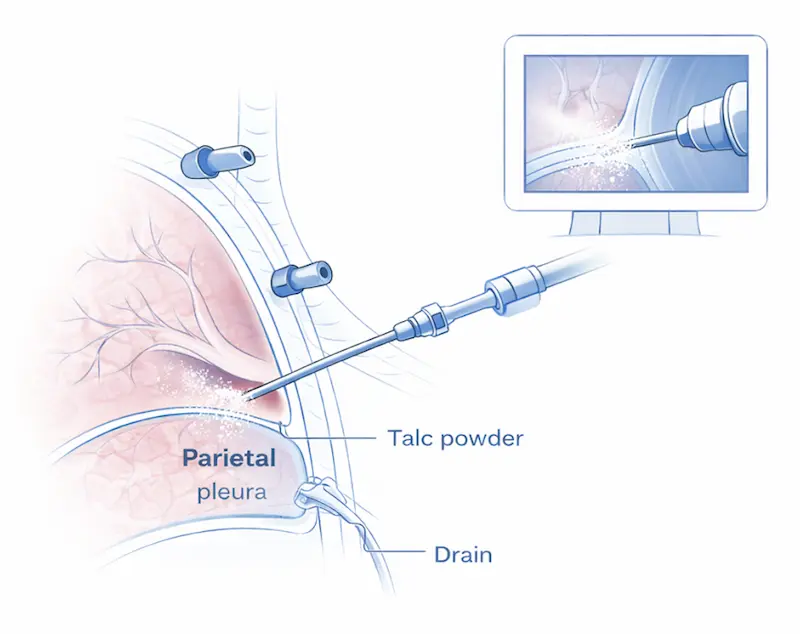
This approach uses safe, effective medications to create the desired pleural adhesion. Professional chemical pleurodesis services typically use one of several proven agents.
The most commonly used and practical option, with success rates often exceeding 90%. Doctors have safely used sterile talc for pleurodesis for decades, and it is entirely different from cosmetic talc.Doctors can often perform medical pleurodesis through a chest tube or chest drain, a procedure called talc poudrage, making it a less invasive option for many patients.
This surgical approach involves physically treating the pleural surfaces to promote adhesion. This procedure is performed by thoracic surgeons during thoracoscopy or thoracotomy, literally abrading or treating the pleural surfaces to encourage them to grow together.
Chemical methods haven’t been successful
Your surgeon can address other issues simultaneously
Your specific anatomy or condition makes a mechanical approach preferable
Please be mindful that pleurodesis is only possible if the lung expands fully. Imagine pleurodesis like glueing two things together; it is only possible if they touch. If the lung does not develop after drainage of the pleural fluid (which we call trapped), we use a semipermanent indwelling pleural catheter. This tiny, soft tube that doesn’t show under your clothes and connects to a special bottle to drain the fluid regularly at home. With ongoing pleural drainage, the space eventually shrinks, and doctors can remove the catheter.
Would you like to discuss whether this approach is suitable for you?
Finding the right thoracic specialist is crucial for successful treatment. Here are two key factors to consider.
Look for surgeons who regularly perform thoracic procedures.
Don’t hesitate to ask about your surgeon’s experience:

Comprehensive lung care teams include not just surgeons, but also pulmonologists, oncologists (if cancer is a concern), specialised nurses, respiratory therapists, and social workers. This team approach ensures all aspects of your care are coordinated and optimised.
If you would value an expert opinion on your condition, a consultation can be arranged below.
Doctors generally recognise these procedures as medically necessary and often cover them with insurance. However, navigating insurance can be complex during an already stressful time.
Diagnostic procedures like biopsies
Therapeutic procedures like pleurodesis
Hospital stays and recovery care
Follow-up appointments and monitoring
If you need help understanding insurance or procedure coverage, our team can guide you.
Experienced nursing staff who specialise in caring for thoracic surgery patients will closely monitor you. Post-operative care includes:
Regular assessment of your breathing and comfort level
Pain medication tailored to your specific needs
Monitoring for any potential complications
Gradual mobilisation to prevent complications and promote healing
Going Home: Most pleural procedures allow you to go home the same day or after an overnight stay.
For comprehensive guidance on pleural effusion management and expected outcomes, see evidence-based pleural effusion treatment guidelines.
Mild to moderate discomfort at incision sites
Some fatigue for the first week or two
Gradual improvement in breathing (this may take several weeks)
Wound check within the first week
Imaging studies to confirm successful healing
Assessment of breathing improvement
Discussion of any ongoing concerns
Successful recovery from any medical procedure involves understanding what’s normal and what requires medical attention:
Mild to moderate discomfort at incision sites
Some fatigue for the first week or two
Gradual improvement in breathing (this may take several weeks)
Contact your healthcare team immediately if you experience:
Severe or worsening chest pain
Significant shortness of breath
Signs of infection (fever, chills, unusual drainage)
Severe nausea or vomiting
Wound check within the first week
Imaging studies to confirm successful healing
Assessment of breathing improvement
Discussion of any ongoing concerns
If you would like to discuss your recovery, procedure, or personalised advice, a consultation can be arranged.
Most patients experience significant improvement in their breathing after successful pleural procedures. While it may take several weeks to feel the full benefits, many patients report breathing better than they have in months or years.
While pleural procedures have high success rates, your healthcare team will discuss backup plans and alternative treatments.
You'll need regular follow-up appointments to monitor your recovery and ensure continued success. The frequency of these visits typically decreases over time as your condition stabilises.
Most patients report that the pleural biopsy is much more tolerable than they expected. Local anaesthesia or sedation ensures comfort during the procedure, and any post-procedure discomfort is typically mild and easily managed.
Success rates for pleurodesis are generally very high, often exceeding 90% for preventing recurrent pleural effusions. Pleurodesis success rates vary slightly depending on the underlying condition and technique used.
Contact me today to schedule your consultation. Your journey to better health starts with a single phone call.