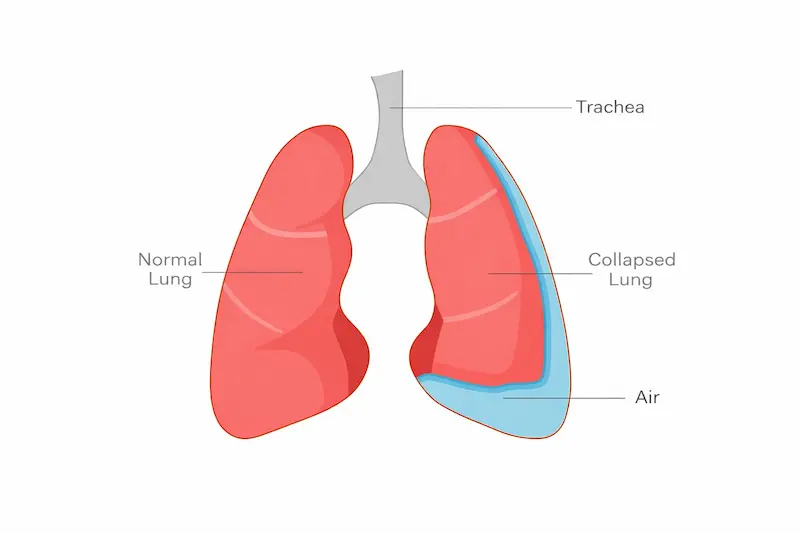
A pneumothorax — often called a collapsed lung — is a condition in which air accumulates in the space between the lung and the chest wall (the pleural space). This air disrupts the normal pressure balance that keeps the lung inflated, causing it to partially or fully collapse. While the idea of a lung collapsing can sound intimidating, understanding pneumothorax causes, symptoms, and treatment options can empower patients to seek timely care, participate meaningfully in decision-making, and recover with confidence.
What pneumothorax is
The different types and causes
Signs and collapsed lung symptoms
This article is written in a simple, jargon-free way to help understanding and includes the critical terminology and evidence-based guidance you need to feel informed and prepared.
At its simplest, a pneumothorax occurs when air leaks into the pleural space — the thin gap between the lung and the inside of the chest wall. Usually, this space is like a vacuum that keeps the lungs expanded as you breathe. When air enters that space, the vacuum effect is lost, and the lung wholly or partially collapses. Imagine a deflating balloon inside a box: if air were to leak into the space around it, the balloon would collapse inward. That’s essentially what happens inside the chest cavity during a pneumothorax.
A pneumothorax may happen suddenly, gradually, or as a result of trauma, an underlying lung condition, or a punctured lung during medical manoeuvres. The severity varies widely depending on how much of the lung has collapsed and what other health issues are involved.
This type occurs without any identifiable trigger or existing lung disease. It’s more common in:
Because it happens in otherwise healthy lungs, it can feel particularly unexpected and alarming.
This type occurs in patients with underlying lung conditions such as:
Here, the pneumothorax results from weakened areas in the lung that rupture and leak air.
Caused by a direct injury to the chest wall — such as a car accident, fall, sports injury, or penetrating trauma — a traumatic pneumothorax can occur alongside other serious complications like rib fractures, hemothorax (blood in the chest cavity), or organ injury.
Traumatic pneumothorax may accompany broken ribs — a significant risk because sharp bone edges can puncture the lung.
This type refers to a pneumothorax caused by medical procedures such as:
Though unintended, it’s a known risk that clinicians can promptly manage.
Unlike other types, tension pneumothorax is a medical emergency. Air enters the pleural space but cannot escape, causing increasing pressure that:
Tension pneumothorax can cause severe hypotension, shock, and severe difficulty breathing. It requires immediate medical attention.
Pneumothorax can occur for reasons that fall into several broad categories:
High-altitude or pressure-changing activities (e.g., scuba diving, aviation), North Tees NHS Trust
Complicated rib fractures
Understanding the cause of your pneumothorax helps define the most appropriate treatment plan. For example, recurrent spontaneous pneumothorax might warrant preventative procedures in addition to acute care.
The hallmark signs of a pneumothorax often appear suddenly and can include: mayoclinic.org+1
Bluish tint to lips or skin (cyanosis) in severe cases
In mild cases, symptoms may start gradually and be more subtle.
If you notice symptoms like these — especially sudden chest pain and breathlessness — seeking urgent medical evaluation is critical, as worsening lung collapse or complications can be life-threatening.

The appropriate treatment for a pneumothorax depends on its severity, cause, symptoms, and the patient’s overall health. In general, options include:
Doctors listen for:
A chest X-ray is the most common initial test. It shows the air outside the lung and how much of the lung has collapsed.
A clinician may order a computed tomography (CT) scan for:
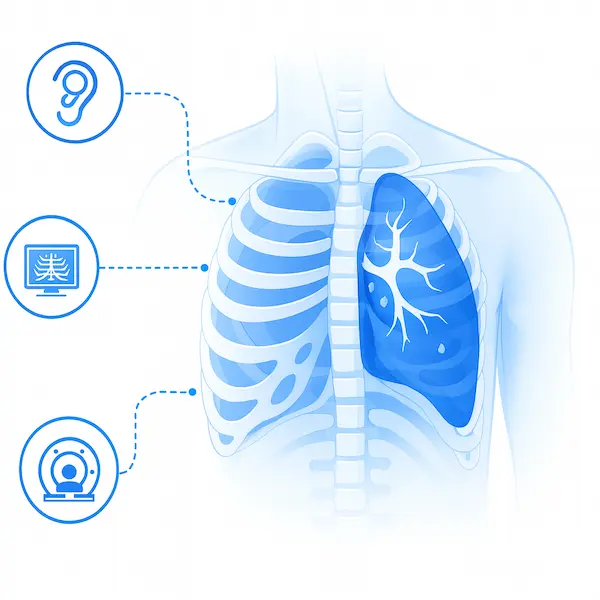
If symptoms are concerning, early imaging helps prevent complications.
The appropriate treatment for a pneumothorax depends on its severity, cause, symptoms, and the patient’s overall health. In general, options include:
For small pneumothoraces with mild symptoms, the body can often reabsorb trapped air on its own. This approach includes:
Careful follow-up ensures that the pneumothorax is not worsening and that symptoms remain stable.
In select cases — particularly in primary spontaneous pneumothorax — a doctor may perform a needle decompression:
This procedure is less invasive and can be an effective first-line intervention in appropriate cases.
Clinicians may place a chest tube (intercostal drain) for a large pneumothorax with significant symptoms, or if conservative management fails:
Chest tube placement is the foundational treatment for many pneumothorax cases — especially traumatic or significant collapses.
Surgeons can perform different surgical procedures to address this issue. Read on for a brief overview.
VATS is a minimally invasive surgical intervention used to:
VATS offers:


Surgeons perform open thoracotomy as a traditional ‘open’ surgery with a larger incision. They rarely need it now, but may use it if VATS isn’t possible. Recovery takes longer, and patients experience more post-op discomfort.
Surgeons may perform a traditional open thoracotomy, although scarce today, for complex or recurrent cases that physicians cannot manage laparoscopically.
VATS is a minimally invasive surgical intervention used to:
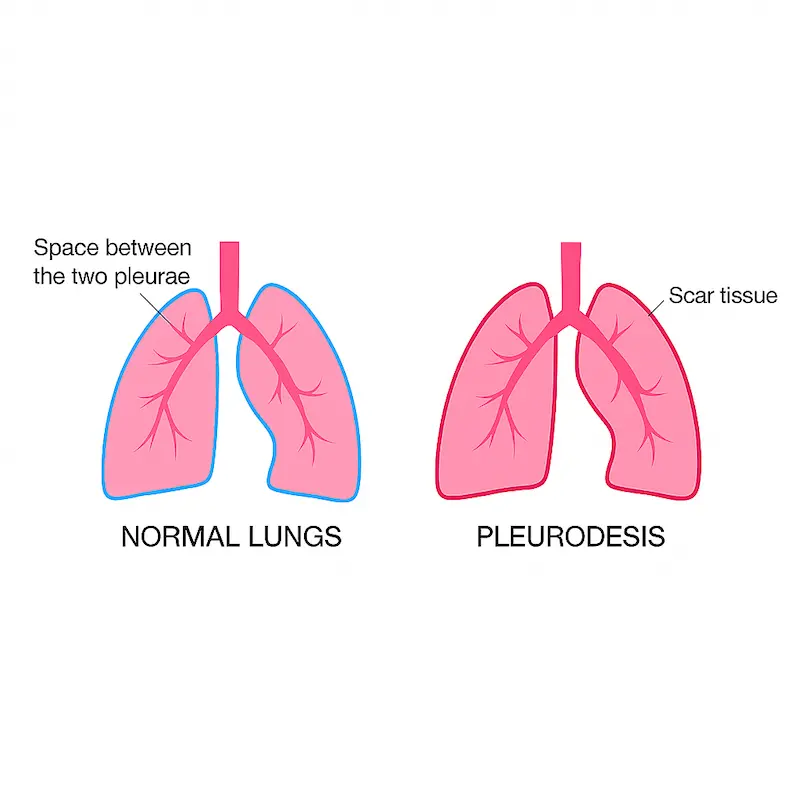
Pleurodesis is often combined with VATS to treat and prevent future episodes simultaneously. Success rates exceed 90% in preventing recurrence.

Most patients recover well, especially when treated promptly and appropriately:
Factors that influence recovery include:
Size of pneumothorax
Cause (spontaneous vs. traumatic)
Presence of underlying lung disease
Smoking status
Quitting smoking, managing chronic lung disease, and avoiding high-risk activities can reduce the risk of recurrence.
Every recovery is individual. A specialist can guide you.
Seek immediate attention if you experience:

Marked shortness of breath
Cyanosis (blue lips or fingertips)
Sudden severe chest pain

Fainting, lightheadedness, or rapid heart rate
These symptoms may signal a progressing pneumothorax or a tension pneumothorax — both of which require emergency treatment.
100 Most Common Patient Questions — Clearly Answered
A pneumothorax can be sudden, painful, and frightening — especially when you don’t know what to expect next.
This free guide answers the 100 most common questions patients ask about pneumothorax, with clear, practical explanations written to inform and reassure you.
You’ll learn:
✔ What pneumothorax really is and why it happens
✔ Which symptoms are urgent and which are not
✔ How doctors diagnose and treat a collapsed lung
✔ What recovery looks like after different treatments
✔ How to reduce anxiety and regain confidence
Written by Marco Scarci, Consultant Thoracic Surgeon
No spam. Instant access. Free.
After a pneumothorax episode, particular lifestyle and medical strategies can help support lung health and prevent recurrence:
Avoid smoking — smoking significantly weakens lung tissue
Discuss safe participation in aviation or pressure changes (e.g., diving)
Work with specialists if you have an underlying lung disease
Maintain regular follow-up if recurrence risk is high
A pneumothorax — while disruptive and sometimes frightening — is now a well-understood condition with a broad array of effective treatment options, ranging from conservative care to advanced thoracic surgery. With timely diagnosis, personalised treatment for pneumothorax, and careful follow-up, most patients recover fully and return to normal life activities.
Whether you’ve just been diagnosed or are seeking to learn more about collapsed lung symptoms and treatment, understanding the types, causes, treatments, and long-term strategies can help you navigate this condition with confidence and clarity.
Expert answers to common questions about thoracic surgery, recovery and what to expect.
Doctors usually recommend surgery after a recurrent pneumothorax, a persistent air leak, or in patients at high risk of recurrence, such as those with underlying lung disease or certain professions.
Yes. Modern techniques such as video-assisted thoracoscopic surgery (VATS) are very safe, with low complication rates and fast recovery for most patients.
Most patients are discharged within 1–4 days after VATS and return to normal activities within 1–2 weeks, depending on overall health.
Surgery significantly reduces the risk of recurrence, primarily when surgeons perform procedures such as pleurodesis.
Contact me today to schedule your consultation. Your journey to better health starts with a single phone call.