For many people, surgery offers the best chance of a complete cure for early-stage lung cancer. The fundamental goal is simple and precise: to remove the cancerous tumour and a small margin of healthy tissue around it, clearing the body of the disease.
Think of it like an expert gardener meticulously removing a single diseased root to ensure the health of the entire plant. Thanks to modern techniques, this process is now safer, less invasive, and allows for a much quicker recovery than in the past.
A Modern Approach to Lung Cancer Surgery
Receiving a lung cancer diagnosis is undoubtedly a daunting experience. However, it's crucial to know that the surgical options available today provide real, tangible hope. The aim of surgery of lung cancer is always to completely remove the tumour along with any nearby tissue that might be affected, giving you the best possible chance of a cure.

Everything we do is guided by a patient-first philosophy. We’ve moved away from the large, open operations of the past and now focus on advanced keyhole techniques. These methods minimise the physical impact on your body, which translates directly to a faster, more comfortable recovery. The progress in this field has been remarkable, making curative surgery a realistic option for more patients than ever.
A Patient's Story of Hope
Let me share the story of Sarah, a 62-year-old teacher diagnosed with early-stage lung cancer. The news came as a shock, bringing fear and uncertainty. She was terrified of a major operation and a long, painful recovery, worrying she’d never get back to her beloved classroom.
Her perspective changed after meeting her surgical team. They explained she was a perfect candidate for a minimally invasive procedure—a keyhole surgery that avoids a large chest opening.
This modern approach made all the difference. Sarah experienced far less pain and was walking the day after her operation. She was home in just a few days, and her return to normal life was faster than she ever imagined. Sarah’s experience is a fantastic real-world example of how today’s surgical advances are transforming lives. You can watch her tell her story below.
Key Benefits of Modern Surgical Techniques
The patient’s journey is at the heart of modern lung cancer care. By using less invasive methods, we can deliver outstanding clinical outcomes while making the entire process far less demanding for you.
Here are some of the key advantages:
- Faster Recovery: With smaller incisions, there's less trauma to your body, meaning you can get back to your normal routine much more quickly.
- Reduced Pain: Post-operative pain is significantly less than with traditional open surgery, reducing the need for strong pain relief.
- Shorter Hospital Stays: Most patients are well enough to go home within 2-3 days, a stark contrast to the week-long stays common with older methods.
- Better Cosmetic Results: The small incisions heal neatly, leaving only minimal scarring.
And the innovation doesn't stop here. The field is constantly moving forward. To get a glimpse of what's on the horizon, have a look at our guide on the future of lung cancer surgery. The ultimate goal is always to improve results while making the treatment journey as smooth as possible for every single patient.
Is Surgery the Right Path for You?
Deciding how to tackle lung cancer is a deeply personal journey, and there’s no single 'right' answer that fits everyone. It's about carefully weighing the options to find the strategy that gives you the best possible chance of a cure. The big question we need to answer together is whether surgery is that strategy for you.
To figure that out, your medical team needs to get a clear picture of the cancer itself. We call this staging, and it’s a crucial first step. Think of it as creating a detailed map that shows us exactly where the cancer is, how big it is, and whether it has started to travel.
- Stage 1: At this point, the cancer is a localised problem, confined to one spot in the lung. It hasn’t spread to any nearby lymph nodes.
- Stage 2: The cancer has begun to move, but only a short distance, perhaps into the lymph nodes within the lung or close by in the chest.
- Stage 3: The journey has become a bit more complex, with the cancer reaching the lymph nodes in the centre of the chest.
- Stage 4: The cancer has travelled much further, spreading to the other lung or to different parts of the body.
This map is vital because it tells us which treatments are most likely to be effective.
The Team Behind Your Decision
You're never making this decision on your own. Your case will be discussed in what’s called a multidisciplinary team (MDT) meeting. This is where a whole group of specialists comes together to pool their expertise and map out the very best plan for you. It’s a true team effort, making sure every angle is covered.
This team usually includes:
- Thoracic Surgeons: Like myself, specialists in surgery of the chest and lungs.
- Oncologists: Experts who manage treatments like chemotherapy and radiotherapy.
- Respiratory Physicians: Doctors who specialise in lung diseases.
- Radiologists: The experts who read and interpret your CT and PET scans.
- Pathologists: The specialists who examine tissue samples to give a precise diagnosis.
We all sit down together, look at your scans, review the biopsy results, and consider your overall health. This collaborative approach is the cornerstone of modern cancer care, ensuring we make the safest and most effective recommendation for you.
"A patient’s journey is at the centre of every decision. By combining our expertise, we can tailor a treatment plan that offers the greatest chance of success while prioritising your quality of life."
When Is Surgery the Best Choice?
For early-stage (Stage 1 and 2) non-small cell lung cancer (NSCLC), surgery is widely considered the gold standard treatment. When the cancer is still contained, removing it completely gives us the highest chance of a lasting cure. For some people with Stage 3 cancer, surgery might also be part of the plan, often after other treatments like chemotherapy.
But the stage of the cancer isn’t the only thing we look at. The MDT also has to consider:
- The Tumour's Location: Is it in a place where a surgeon can safely get to it and remove it completely?
- Your Overall Fitness: Are you strong enough for an operation? We'll look closely at your heart and lung function to make sure you can handle the surgery and recover well.
It's great news that thanks to huge advances in surgical techniques, more people are now able to have surgery than ever before. We're seeing this in the numbers, too. In a recent year, a record 7,018 people with NSCLC in England had surgery with the aim to cure, which is a 20% increase on the year before. This shows just how much confidence has grown in surgical outcomes, driven by better detection and less invasive procedures. You can read more about these encouraging trends in the latest national lung cancer audit report.
Ultimately, the final recommendation will always be tailored to you, balancing the powerful potential of surgery against your unique health circumstances to find the path that leads to the best possible outcome.
Comparing Keyhole and Open Lung Surgery
When you and I sit down to discuss your operation, we’ll focus on two key questions. First, how much of the lung needs to be removed to get rid of the cancer completely? And second, what’s the best way for me to get there?
Answering the first question is all about making sure we remove all the cancerous cells while preserving as much healthy lung as possible. Depending on the size and location of your tumour, we might consider one of several procedures:
- Wedge Resection: Think of this like carefully cutting a small, bruised spot out of an apple. We remove a small, wedge-shaped piece of lung tissue that contains the tumour, leaving the vast majority of the healthy lung untouched.
- Segmentectomy: This is a step up from a wedge resection. Here, we remove a slightly larger, anatomically distinct portion of the lung lobe, called a segment. It’s a good balance between removing enough tissue and saving lung function.
- Lobectomy: This is the most common and often the standard operation for early-stage lung cancer. Your right lung has three lobes and your left has two; a lobectomy involves removing one of these entire lobes.
Once we’ve decided on what to remove, the next part of our conversation is about how we do it. This is where surgical techniques have taken a giant leap forward in recent years.

From Open Surgery to Keyhole Precision
For a long time, the only option for lung surgery was a thoracotomy, or what we call open surgery. It involves a long incision across the side of the chest and spreading the ribs apart to give the surgeon direct access. It’s effective, of course, but it’s also a major procedure that causes significant trauma to the chest wall, which naturally leads to more pain and a longer, tougher recovery.
Thankfully, things have changed. Today, the vast majority of lung cancer operations are performed using minimally invasive surgery (MIS), which you’ll often hear called ‘keyhole’ surgery. Instead of that large cut, we use just a few small incisions. No rib spreading required.
"I believe strongly that the best patient outcomes are achieved by combining surgical expertise with compassion, innovation, and close collaboration across specialties. My goal is to bring patients not only the most advanced techniques in thoracic surgery, but also the reassurance that they are never facing the challenges ahead alone."
The two main types of keyhole surgery I perform are:
- Video-Assisted Thoracoscopic Surgery (VATS): I insert a tiny, high-definition camera (a thoracoscope) and specially designed instruments through a few small cuts. I then watch a monitor that gives me a crystal-clear view inside the chest, allowing me to perform the operation with incredible precision.
- Robotic-Assisted Thoracic Surgery (RATS): This is the most advanced evolution of keyhole surgery. I sit at a console in the operating theatre, controlling state-of-the-art robotic arms that hold the instruments. This technology gives me a magnified, 3D view and a level of dexterity and control that surpasses what the human hand can do alone.
A Patient's Story of Choosing Keyhole Surgery
David, a 68-year-old retired engineer, was understandably apprehensive when I told him he needed a lobectomy. He had a vivid memory of his father going through open lung surgery decades earlier and recalled the long, painful recovery that followed. His biggest fear was losing his independence and not being able to enjoy the retirement he’d worked so hard for.
During our consultation, I explained just how much the world of surgery had moved on. We reviewed his scans together, and I was able to tell him he was a perfect candidate for a robotic-assisted lobectomy. I showed him how, instead of a large incision, we’d use four small ones, each no bigger than a keyhole.
The difference was night and day. David’s surgery went perfectly, and he was up and walking on the ward the very next day. His pain was easily managed, and he was ready to go home after just two days in hospital. A few weeks later, he was back to his daily walks and tinkering in his workshop, feeling hugely relieved and grateful for a recovery he never thought was possible.
Comparing Lung Cancer Surgical Approaches
The choice between open and keyhole surgery is one we’ll make together, based entirely on your individual situation—the specifics of your cancer and your general health. That said, for most patients I see, the advantages of a minimally invasive approach are undeniable.
The table below gives you a clear, side-by-side look at the differences.
| Feature | Open Surgery (Thoracotomy) | Minimally Invasive Surgery (VATS/Robotic) |
|---|---|---|
| Incision Size | One long incision (10-20 cm) | Several small incisions (1-3 cm each) |
| Post-Op Pain | Significant; often requires strong pain relief | Mild to moderate; managed with simpler medication |
| Hospital Stay | Typically 5-7 days or longer | Typically 2-3 days |
| Recovery Time | 6-8 weeks or more to return to normal activities | 2-4 weeks to feel significantly better |
| Blood Loss | Higher potential for blood loss | Minimal blood loss |
| Complications | Higher risk of infection and pneumonia | Lower risk of post-operative complications |
My goal is always to use a keyhole approach, but my absolute priority is your safety. In a very small number of cases, it might become necessary to convert to an open procedure during the operation to ensure the best possible outcome. This is a rare event, but it’s an important safety net. You can learn more about the reasons for a VATS conversion to open surgery in our detailed article.
A Patient's Journey Through Lung Cancer Surgery
Sometimes, a real story makes things clearer than any statistic ever could. Let's walk through the experience of someone who has been where you are now—someone who faced a lung cancer diagnosis and found their way back to health through modern surgery. This is a story of hope, but also a realistic look at what the process is like.
From Diagnosis to a Plan
Meet Michael, a 65-year-old retired accountant from London. It all started with a persistent cough that led to a chest X-ray and, eventually, scans confirming a small, early-stage tumour in his right lung. The news was, of course, a huge shock. Michael’s mind immediately jumped to the worst-case scenarios: a massive operation, debilitating pain, and a long recovery that would keep him from his grandchildren.
That first consultation was the turning point. We sat down, and before diving into clinical details, we just talked. I listened to his fears and answered every single question he had. I explained how we could use a keyhole approach—specifically robotic surgery—to remove the tumour through a few tiny incisions. Showing him the 3D visuals of how it worked helped replace that initial fear with a sense of control and understanding.
The Surgery Itself
Michael’s surgery was scheduled at a leading London hospital just a week later. From the pre-operative checks to meeting the reassuring anaesthetic team, the entire process was designed to be as smooth as possible. When he woke up, his first surprise was the lack of pain. Instead of a large, uncomfortable wound, he just had a few small dressings on his side.
The very next day, Michael was up and walking the corridors with the help of our physiotherapist. He was genuinely amazed at his own progress. After just two nights in the hospital, he was discharged and went home with a clear, manageable plan for his recovery.
"I thought my life was over when I heard the word 'cancer'. But the care I received was incredible. The surgery was nothing like I feared, and the recovery was faster than I could have ever imagined. I feel like I've been given a second chance." – Michael, Patient.
Getting Back to Normal Life
At home, Michael’s recovery continued to be swift. He stuck with his breathing exercises and gradually started moving more, feeling stronger with each passing day. Within just a few weeks, he was back to taking his grandchildren to the park, without feeling held back by his operation. His story is a powerful example of how minimally invasive surgery of lung cancer can produce excellent results with very little disruption to your life.
This focus on advanced techniques is changing the patient experience across the UK. Innovation is driving better survival rates and a higher quality of life. In fact, one-year survival rates have hit a record 50% in England, largely thanks to better treatments for early-stage disease where surgery is most effective. Private innovation is also pushing things forward, often cutting hospital stays by 25% compared to national averages. You can read more about these trends in the UK lung cancer surgery market on futuremarketinsights.com.
Michael's journey isn't an isolated case; it's fast becoming the new standard of care.
From Your First Consultation to Your Full Recovery: What to Expect
Facing lung cancer surgery can feel overwhelming, but understanding the journey ahead can make a world of difference. The entire process, from your first assessment to the day you're back on your feet, is a carefully planned pathway. It’s designed to prepare you physically and mentally for the best possible outcome and support you every step of the way.
To help you visualise this, here’s a typical patient journey, showing how each stage flows logically into the next.
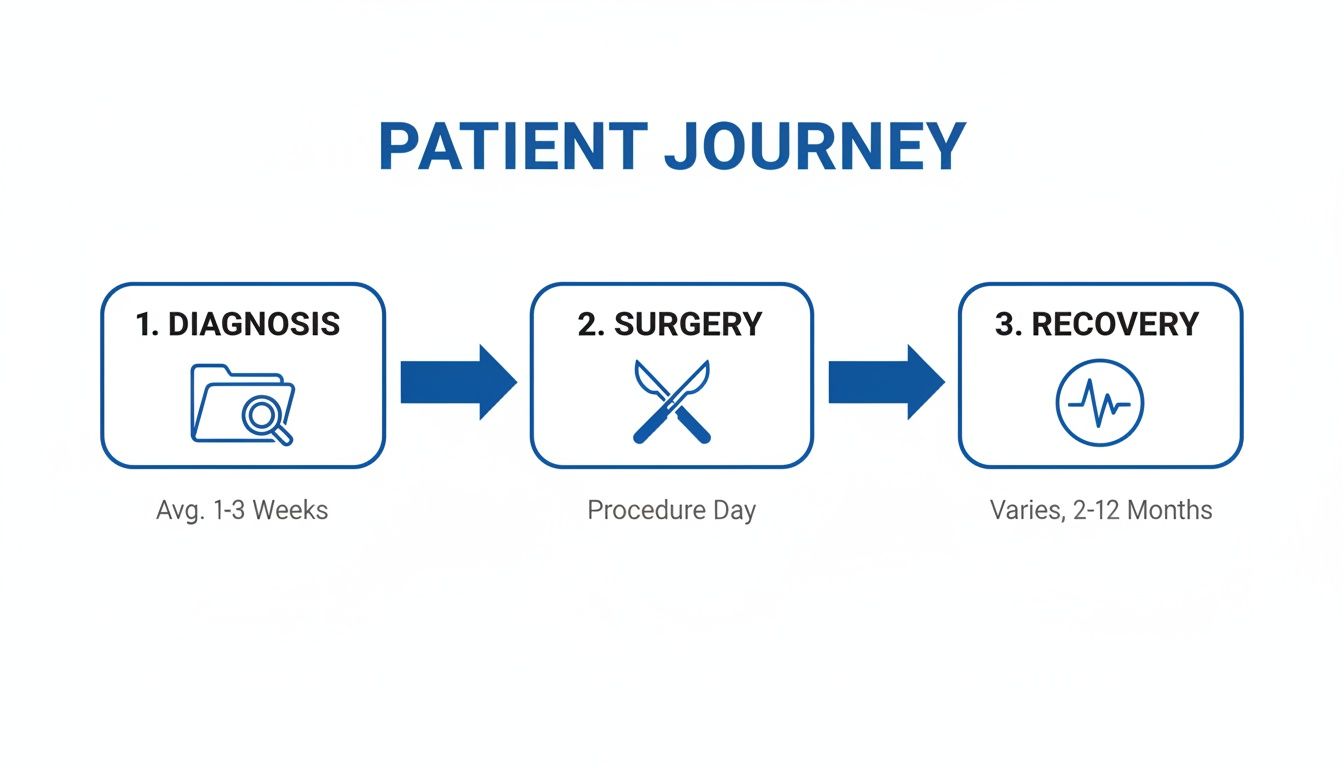
This map shows how we move from diagnosis and preparation, through to the operation itself, and finally, into a structured recovery phase that gets you back to your life.
The Pre-Operative Assessment: Getting You Ready for Surgery
Before we can proceed with any operation, a thorough pre-operative assessment is essential. This isn't just a box-ticking exercise; it's a vital step to ensure your body is ready for the procedure and to minimise any potential risks.
We’ll run a few key checks, including lung function tests like spirometry. This tells us exactly how well your lungs are working and confirms you have plenty of respiratory reserve to recover well after surgery. You'll also have standard blood tests and an ECG to get a clear picture of your heart health. If you'd like to understand this stage in more detail, we have a comprehensive guide on the lung cancer surgery assessment.
"I had a lot of anxiety about the operation itself, but the pre-assessment was incredibly reassuring. The team explained everything, from the anaesthesia to the first few days of recovery, so I knew exactly what to expect. It made a huge difference to my mindset." – A Former Patient.
This is also your chance to meet the anaesthetist. They’ll review your medical history, discuss the anaesthesia plan, and answer any questions you have, ensuring you feel completely informed and at ease.
Enhanced Recovery After Surgery (ERAS): A Modern Approach to Healing
Your recovery isn't something that starts after surgery; it begins long before. We follow a modern, evidence-based pathway called the Enhanced Recovery After Surgery (ERAS) programme. Think of it as a complete care philosophy aimed at getting you back to normal faster and more comfortably.
ERAS isn’t one single thing but a combination of many small, important details:
- Pre-Surgery Nutrition: We make sure you’re well-nourished before the operation, which gives your body the fuel it needs to heal efficiently.
- Smarter Pain Management: Our goal is to keep you comfortable using a multi-pronged approach that minimises the side effects of strong painkillers.
- Getting You Moving: We encourage you to get up and about as soon as it's safe. Early mobilisation is one of the best ways to prevent complications and speed up recovery.
This holistic approach has been proven to shorten hospital stays and lead to better outcomes, making your recovery journey much smoother.
Your Hospital Stay and the First Few Days
Once your surgery is complete, you'll spend a short while in a recovery area before being moved to the ward. From the moment you wake up, our dedicated nursing and physiotherapy teams will be there to guide and support you.
You will most likely have one or two chest drains. These are small, thin tubes that help remove any air or fluid from your chest, allowing your lung to re-expand and heal properly. We typically remove these within 24 to 48 hours.
We’ll manage your pain very carefully, not just for comfort, but to ensure you can breathe deeply and start moving around. Thanks to modern keyhole techniques, most patients are ready to head home within just two to three days.
Settling in for Recovery at Home
Leaving the hospital is a big milestone, but your recovery journey continues at home. It's completely normal to feel tired for a few weeks, so the most important thing is to listen to your body and rest when you feel you need to.
The breathing exercises you learned in the hospital are a crucial part of your daily routine. They help keep your lungs clear and working well. You’ll be encouraged to gradually increase your activity, starting with short walks and slowly building back to your normal routine. For more in-depth advice, this resource offers practical guidance for recovering from surgery at home.
Accessing Fast-Track Private Lung Cancer Care
When you’re facing a lung cancer diagnosis, the waiting is often the hardest part. The uncertainty can be incredibly stressful, and for many people, the need to act quickly feels overwhelming. This is where private care can make a real difference, offering a direct and rapid path from your diagnosis to the operating theatre, sometimes in as little as one week.
The whole point of this fast-track approach is to reduce that anxiety and get your treatment started without unnecessary delays. We provide a highly personal, concierge-level service. This means you get direct access to your surgeon and we can arrange consultations—either virtual or in-person—at your convenience. All treatment is carried out in London's premier private hospitals, so you can be confident you're receiving exceptional care in a first-class environment.
A Patient's Story of Swift Action
Let me share the story of a gentleman who got in touch with us right after his lung cancer diagnosis. He was understandably worried about potential NHS delays and the toll this uncertainty was taking on his family. He knew he wanted the best possible care, and he wanted it fast.
From that very first phone call, we set up a virtual consultation for the next day. After I reviewed his scans and we discussed his options for keyhole surgery of lung cancer, we were able to book his procedure for just five days later. The sense of relief he felt was immense; a clear plan was in place. This is what we do—we offer not just surgical expertise, but also genuine peace of mind when it matters most.
How Private Care Works
We make our care accessible in a few different ways. Many of our patients self-fund their treatment, while others use private medical insurance from providers like Bupa, AXA, or Aviva.
If you have insurance, it’s really important to look into your coverage thoroughly, especially when it comes to understanding medical conditions and policy exclusions in private insurance. We can help guide you through the process and also offer financing options to make sure timely treatment is always within reach.
This streamlined pathway is also designed for GPs and physicians who refer their patients to us. A simple referral process and our commitment to working collaboratively means your patients get the prompt, specialist attention they need. We’ve found that focusing on a patient's overall fitness, rather than just their age, leads to the best outcomes. This approach is backed by solid research; UK screening trials have shown that even patients up to age 80 who are fit for surgery have excellent survival rates, with a four-year mortality of just 16%.
Your Questions Answered
It's completely normal to still have questions buzzing around your head, even after going through all the details of the surgery and what recovery looks like. This section is here to give you clear, straightforward answers to some of the most common things patients worry about when they're considering lung cancer surgery.
What Are the Real Risks Involved?
Look, every operation has some element of risk—there's no getting around that. But it's important to know that modern lung surgery, especially in experienced hands, is safer than it has ever been.
Most of the potential issues we see are manageable things. For example, a prolonged air leak, which just means the lung takes a bit longer to fully seal itself, or a chest infection that we can treat effectively with antibiotics.
Serious complications are genuinely rare, and that's especially true when you're being treated by a specialist team in a centre that does this work day in, day out. We are meticulous about minimising these risks, from detailed pre-op checks right through to the precision of the surgery itself. Your safety is, and always will be, our number one priority.
How Long Will I Be in Hospital?
This is where the advances in minimally invasive surgery have completely changed the game. For a keyhole operation like a VATS or robotic lobectomy, most of our patients are now home in just two to three days.
It’s a world away from the week or more that was standard with older, open operations. Our whole focus is on getting you back to the comfort of your own home as soon as it’s safe and you feel ready to continue your recovery there.
A Patient's Story: Life After Surgery
I often think of a patient of mine, David. He was a passionate golfer, and his biggest fear wasn't the cancer itself, but that surgery would rob him of his favourite pastime. He underwent a robotic-assisted segmentectomy, and his recovery was remarkable. He felt tired for a few weeks, of course, but he stuck to his physiotherapy exercises religiously.
About six weeks after his operation, he sent me a video. It was him, on the driving range, taking his first gentle swing. The sheer joy on his face said it all. His story is a powerful reminder that we don't just do this to remove cancer—we do it to give you your life back.
"I honestly thought I'd be fragile for months, but the recovery was much faster than I expected. Getting back to the golf course felt like a massive victory, not just over cancer, but over the fear of what surgery would mean for my life."
Will I Be Able to Live a Normal Life?
For the overwhelming majority of patients with early-stage lung cancer, the answer is a definite yes. The whole point of a lobectomy (removing a lobe) or a segmentectomy (removing a smaller segment) is to get rid of the cancer completely while leaving as much healthy lung as possible.
Most people find that once they're past the first few weeks of recovery, their breathing is absolutely fine for all normal daily activities. You can get back to work, enjoy your hobbies, and lead a full, active life. You might notice some breathlessness when you really exert yourself at first, but this almost always improves as your body adapts.
How Do I Get a Second Opinion?
Asking for a second opinion is a very normal and sensible thing to do. It can give you peace of mind that you're on the right track, or perhaps offer a different perspective you hadn't considered.
It's a simple process. You can ask your GP or your current specialist to refer you to another surgeon. If you're considering private care, you can also contact a specialist like me directly. All we need is access to your recent scans and medical history to review your case and give you a thorough, informed opinion.
If you have more questions or wish to discuss your options for fast-track private care, please get in touch with Marco Scarci Thoracic Surgery. Arrange your consultation today.