If you've suffered a painful chest injury, one of the first questions on your mind will likely be, "What will an X-ray of my broken ribs actually show?" In any UK A&E, a chest X-ray is the go-to first step for a suspected rib fracture. But it’s important to understand that this initial scan is just a snapshot, not the full story.
Your First Look at a Broken Rib X-Ray

When you're sitting in A&E with agonising chest pain, the wait for those X-ray results can feel endless. That black-and-white image holds the first vital clues to what's going on, but reading it properly is more of an art than you might think.
This guide will walk you through what those initial scans can tell us, where they fall short, and what happens next. The goal is to give you a clearer understanding of your own medical journey so you can feel more in control of your recovery.
Understanding the Initial Diagnosis
A standard X-ray is brilliant at picking up obvious, displaced breaks—where the two ends of the bone have clearly shifted out of alignment. The problem is, it often misses injuries that are more subtle.
Here’s what you need to bear in mind about that first scan:
- Hairline Fractures: These are tiny, fine cracks in the bone that are often too small to be visible on an initial X-ray.
- Cartilage Injuries: The flexible cartilage connecting your ribs to your breastbone (sternum) is soft tissue, so it doesn't show up on an X-ray at all. Any damage here will be completely invisible.
- Location Matters: Some ribs are tucked away behind organs like the heart or diaphragm, making them incredibly difficult to see clearly on a two-dimensional image.
Blunt chest trauma involving multiple fractured ribs is a serious issue, accounting for a significant 15% of all United Kingdom trauma centre admissions. This translates to approximately 5,550 cases each year across the UK.
When Your Pain Doesn't Match the Scan
It's a very common scenario: you’re in severe pain, but the doctor comes back and says your X-ray is "clear." This can be incredibly confusing and frustrating. It absolutely does not mean your pain isn't real; it just means the standard X-ray wasn't the right tool for the job in this case.
This is precisely why doctors will often diagnose a "clinical fracture" based on your symptoms alone. Recognising the common broken rib symptoms is vital for both you and your medical team. If the pain is severe and doesn't improve, it’s a strong signal that further investigation, usually with a CT scan, is needed to get the full picture and make sure your treatment is on the right track.
A Patient's Journey: Why the First Scan Isn't Always the Full Story
Sometimes, the best way to understand a medical issue is to walk in someone else's shoes. A patient's experience can highlight just how crucial it is to listen to your body when the initial tests don't match your symptoms.
One of my patients, a gentleman who'd had a nasty fall, went through this exact scenario. His story, which you can see in the video below, is a powerful example of why an x-ray of broken ribs is often just the beginning of the diagnostic process.
He came to the emergency room with severe chest pain. The initial x-ray was done, and the report came back showing only a couple of minor fractures. He was sent home with standard advice: rest and take painkillers. But his pain didn't improve—it got worse. He was struggling to breathe, unable to sleep, and knew that something was seriously wrong. This disconnect between the 'minor' diagnosis and his extreme pain prompted him to seek a specialist opinion.
When an X-Ray Can't See Everything
This patient's experience is far from unusual. An x-ray is a flat, two-dimensional image, and it's surprisingly easy for it to miss fractures, especially if they aren't displaced or are hidden behind other organs. Trusting his instincts, he sought a second opinion where a more detailed imaging plan was put in motion.
This time, a CT scan was ordered. Unlike an x-ray, a CT scanner takes a series of detailed, cross-sectional pictures, building a 3D-like view of the bones and soft tissues. The results were a revelation, and they finally explained the intensity of his pain.
The CT scan revealed not one or two, but seven fractured ribs, several of which were significantly displaced—a detail completely missed by the initial x-ray. It also showed a dangerous build-up of fluid around his lung.
The Power of an Accurate Diagnosis
This gentleman's story is a powerful reminder that you are the ultimate expert on your own body. While an x-ray is a crucial first step, it’s not infallible. If your symptoms feel far more severe than your initial scan suggests, it's absolutely right to advocate for a deeper look. A precise diagnosis, in his case leading to surgical fixation, was the bedrock of a proper recovery plan.
As patients move through this process, clear and accurate medical records are essential. Innovations in streamlined healthcare documentation are making this much easier, ensuring every detail of a complex diagnosis is captured correctly.
His journey teaches a vital lesson: listen to your body. If the pain and symptoms don't align with the initial findings, don't be afraid to push for a clearer diagnosis.
Decoding the Black and White: What Doctors See on Your Scan
To the untrained eye, an X-ray of broken ribs can look like a confusing jumble of grey and white shapes. For a radiologist or surgeon, though, it’s a detailed map. They’re hunting for specific clues that reveal exactly what’s going on inside your chest.
The most obvious sign of a break is a fracture line. Think of it like a crack running through a smoothly painted white wall – it’s a thin, dark line that interrupts the otherwise solid, white surface of the bone. Sometimes this line is wide and obvious, but often it’s a faint hairline that takes a highly trained eye to spot.
From Simple Cracks to Misaligned Breaks
Beyond just finding a crack, doctors are also looking for displacement. This is a crucial detail that tells us if the two broken ends of the rib are still neatly aligned. A non-displaced fracture is like a cracked plate that hasn't shifted; a displaced one is where the pieces have moved apart. The more displaced a fracture is, the higher the risk of it puncturing a lung or damaging other internal structures.
An X-ray is the essential first step, but its limitations are well known. A "clear" scan doesn't always mean you don't have a fracture, which can be incredibly frustrating when you're in severe pain. It simply means that particular tool couldn't see the injury.
Why X-Rays Sometimes Miss the Mark
It's a surprisingly common scenario: you’re in agony, convinced something is broken, yet the X-ray comes back clear. This doesn't mean your pain isn't real. In fact, studies have shown that initial chest X-rays, long the standard in UK A&E departments, miss a shocking number of rib fractures.
Some research suggests up to 45-50% of fractures aren't visible on the first scan. This is a major reason clinical guidelines are constantly being updated to improve patient care. You can read more about these findings in the published research on imaging limitations.
So, why do these fractures hide?
- Location, Location, Location: Ribs tucked away behind the heart, diaphragm, or other dense organs are notoriously difficult to see on a flat, 2D image.
- Hairline Cracks: Tiny, non-displaced fractures might only become visible a week or two later, when the body starts forming a healing callus around the break.
- Cartilage Injuries: The flexible cartilage that connects your ribs to your breastbone (sternum) is completely invisible on an X-ray. You can have a painful tear there, and the scan will look perfectly normal.
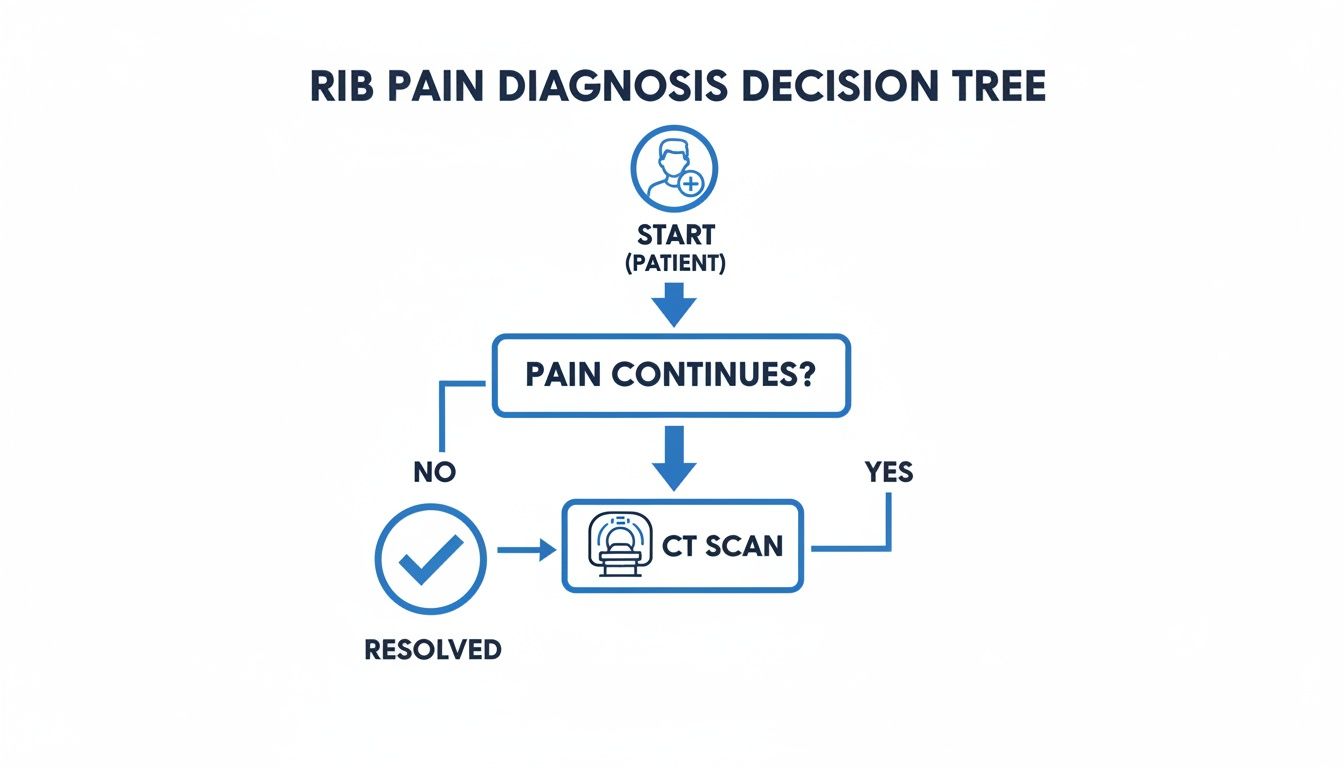
This decision tree shows the typical diagnostic path a doctor might follow when rib pain continues despite a clear initial check.
The key takeaway here is that persistent, severe pain should always trigger a closer look. More often than not, this means moving on to a more powerful imaging tool, like a CT scan, to get the full picture.
Comparing Imaging Scans for Rib Fractures
When a simple X-ray doesn't provide all the answers, your doctor has other tools at their disposal. Each type of scan has its own strengths and weaknesses, and the choice depends on what they need to see. This table breaks down why one might be chosen over another.
| Imaging Type | What It's Best For | Key Benefit | Main Limitation |
|---|---|---|---|
| X-Ray | Quick initial assessment, identifying obvious and displaced fractures. | Fast, widely available, and uses a low dose of radiation. | Misses hairline fractures, cartilage damage, and internal injuries. |
| CT Scan | Getting a highly detailed, 3D view of complex fractures and checking for organ damage. | The "gold standard" for accuracy – shows bone, organs, and blood vessels clearly. | Higher radiation dose and more expensive than an X-ray. |
| Ultrasound | Examining soft tissue, cartilage injuries, and checking for fluid around the lungs. | No radiation, excellent for soft tissue, and can be done at the bedside. | Less effective for seeing bone details deep within the chest. |
Ultimately, the goal is to match the right imaging technique to your specific symptoms and injury. A CT scan is often the next logical step when there's a strong suspicion of a fracture that an X-ray missed, or if there's any concern about complications like a punctured lung.
Identifying Serious Complications Beyond the Break

When we look at an X-ray of broken ribs, we're searching for more than just the number of cracks. The real priority is spotting signs of serious internal damage. This is what can elevate a painful injury into a life-threatening emergency and explains why a hospital stay is sometimes essential, even if the injury seems minor at first.
One of the most immediate dangers we look for is a pneumothorax, which is a collapsed lung. It happens when the jagged edge of a broken rib pierces the lung, allowing air to escape into the chest cavity and build up pressure. On an X-ray, this shows up as a dark, empty-looking space where healthy lung tissue should be. It’s a clear signal the lung has deflated and can't do its job. For a deeper look at how this is managed, you can read our guide on how to treat a pneumothorax.
The Most Severe Injuries
Another major concern is a condition called flail chest. This is a particularly nasty injury where at least three ribs in a row are broken in two or more places. This creates a segment of the chest wall that is completely detached from the rest of the ribcage.
The result is paradoxical movement. When the patient breathes in, this "flail" section gets sucked inwards, and when they breathe out, it bulges outwards. This isn't just incredibly painful; it critically impairs their ability to breathe properly.
"I remember one patient, a motorcyclist, who came in after a collision. His initial X-ray showed multiple breaks, but the real concern was the flail segment we identified. His breathing was unstable, and we knew immediate, specialised care was essential to stabilise his chest wall and prevent respiratory failure."
This patient’s story really brings home why we have to be so vigilant. Blunt trauma to the chest is notorious for causing these kinds of dangerous secondary injuries.
A major UK-wide analysis by the Trauma Audit and Research Network (TARN) looked at 5,680 patients and found that flail segments occurred in 14.6% of cases. Even more common was pneumothorax, present in a staggering 44.3%.
Beyond what an X-ray shows, clinicians often use pulmonary function test interpretation to get a clearer picture of how badly the lungs are affected. That same TARN study found lung contusions (bruising of the lung tissue) in 36.1% of patients, which is another serious complication that we have to monitor very closely.
Your Action Plan for Pain Management and Recovery
Once you're home from A&E, the real work of recovery begins. Getting this stage right is about more than just managing your comfort levels; it's absolutely vital for preventing some pretty nasty complications. Your number one job is to get the pain under control so you can breathe properly.
The biggest danger with a broken rib isn't actually the bone itself. It's the cascade effect that follows. When every breath is agony, you instinctively start taking shallow, guarded breaths. This stops your lungs from fully expanding and clearing out mucus, which can quickly lead to a chest infection or even pneumonia.
So, think of pain relief as your first and best line of defence. This isn't the time to "tough it out"—it's about giving your body the ability to do what it needs to do to heal.
Mastering Pain Control and Breathing
The NHS approach is usually the best place to start: a simple but effective pain relief plan. This typically means alternating paracetamol with an anti-inflammatory like ibuprofen. The trick is to take them regularly, like clockwork. Don't wait for the pain to ramp up before you take a dose; staying ahead of it makes a world of difference.
With the pain dialled down, you can start focusing on your breathing. You don't need any fancy equipment for this.
- Deep Breaths: Make a point of taking five to ten slow, deep breaths every hour you're awake. Inhale as much as you can without sharp pain, hold it for a moment, and then exhale slowly.
- Supported Coughing: You have to cough to keep your lungs clear. It will hurt, but you can make it much more bearable. Hug a pillow tightly against your injured side to brace the area, and then give a firm cough.
"The single most important aspect of non-operative rib fracture management is adequate pain control. This allows for deep breathing and effective coughing, which are essential to prevent the lungs from collapsing or developing pneumonia."
Creating a Healing Environment
While your body needs rest to knit those bones back together, lying completely still is not the answer. Gentle movement is key. Just walking around the house a few times a day helps with blood flow and keeps your lungs working. You're looking at a healing timeline of around six weeks for the bone itself, but be prepared for some pain to stick around for a while longer.
Sleep is often the biggest battle. Lying flat can feel impossible.
- Try sleeping propped up: Build a ramp with pillows to keep your upper body elevated. A semi-upright position often takes the pressure off.
- Consider a recliner: If you have an armchair that reclines, it can be a lifesaver. It provides great support and makes getting in and out of it far less painful.
Patience really is a virtue here. For those with more complex fractures needing surgery, the journey is a bit different. You can get a clearer picture of that process by reading about post-surgery care for rib fractures. By taking an active role in managing your pain and breathing, you put yourself firmly in control of your own recovery.
When It's Time to Call in the Specialists
Most of the time, a few fractured ribs mean a painful but straightforward recovery at home with rest and good pain relief. But some injuries are a different beast altogether, and knowing when to seek specialist help is vital for avoiding serious trouble down the line.
I remember a 65-year-old gentleman who came to see me after a nasty fall from a ladder. He’d been to his local A&E, diagnosed with a few fractures, and sent home. But over the next 48 hours, things went downhill fast. The pain became unbearable, and he felt more and more breathless with every passing hour. This is a classic warning sign. He did exactly the right thing and came straight back to hospital. A CT scan revealed what the initial x ray of broken ribs hadn't fully shown: his fractures were far more displaced, and his breathing was dangerously compromised.
Red Flags That Mean "Go Back to Hospital"
If you've been sent home with rib fractures and any of these symptoms crop up, you need to return to A&E immediately. Don't wait it out.
- Severe Shortness of Breath: If you feel like you just can't get a proper breath in, it's a medical emergency.
- Pain That's Out of Control: Your pain should be manageable with the medication you were given. If it's getting worse, something isn't right.
- A High Fever or Shaking Chills: This is a major sign that a chest infection, like pneumonia, could be setting in.
- Feeling Confused or Unusually Drowsy: This can be a sign of dangerously low oxygen levels.
Getting a Referral to a Thoracic Team
In complex cases like the gentleman who fell, a referral to a specialist thoracic team is the next logical step. This typically happens when someone has multiple displaced fractures, pain so bad they can't take a deep breath, or the tell-tale signs of a flail chest. Within the NHS, these severe injuries are usually handled at Major Trauma Centres, where the right expertise and equipment are on hand.
When you're dealing with multiple, severe fractures, surgical fixation—often called rib plating—can be a game-changer. By stabilising the chest wall with small plates, the procedure can dramatically reduce pain and help you get back to breathing normally much, much faster.
For those who want to explore this kind of advanced care more quickly, private options can offer a direct route. A private specialist thoracic surgeon can provide a rapid consultation to see if surgical fixation is the right choice for you, helping you bypass potential delays and get on the road to recovery sooner.
Common Questions About Broken Rib X-Rays
Navigating the aftermath of a chest injury can be a confusing and painful experience, especially when what you're feeling doesn't seem to line up with the initial X-ray results. Let's tackle some of the most common questions people have after an injury.
I recently saw a patient who had been in a car accident. She was in absolute agony, yet the A&E team told her the initial chest X-ray showed nothing. They suspected a 'clinical fracture' based purely on her symptoms, but with no clear image to back it up, she was left feeling frustrated and uncertain about what was really going on.
A few days later, her pain got so bad she could barely take a deep breath – a major red flag. We fast-tracked her for a CT scan, which finally gave us the full picture: two very subtle, non-displaced fractures that were completely invisible on the first scan. This not only validated her pain but allowed us to put a proper pain management plan in place and head off a potential chest infection.
Why Does My Chest Still Hurt if the X-Ray Was Clear?
This is an incredibly common scenario, so you're not alone. A standard chest X-ray can miss up to half of all rib fractures. They're particularly poor at picking up fine hairline cracks, injuries to the rib cartilage (which doesn't show up on X-ray), or fractures that aren't out of alignment.
This is why a doctor might diagnose a 'clinical' fracture based on your symptoms alone. The pain from deep bruising or torn cartilage is just as severe as a clean break and needs to be managed just as carefully. The priority is always to control the pain so you can breathe properly and prevent complications like pneumonia.
How Long Does It Take for Broken Ribs to Fully Heal?
For the bones themselves, you're looking at a healing window of about six weeks. That's the typical timeframe for the bone to knit back together.
However, the surrounding pain in the muscles and nerves can linger for much longer, often for several months. Your recovery really depends on your age, your general health, and how severe the injury was. It is absolutely vital to avoid any strenuous activity or heavy lifting during that initial six-week period to give the fractures the best chance to heal without disturbance.
What Are the Warning Signs of Pneumonia After a Rib Injury?
Pneumonia is a genuine risk because the pain from the injury stops you from taking deep breaths and clearing your lungs effectively. You must seek urgent medical care if you start to notice any of these signs:
- A new or worsening cough, especially if you're bringing up coloured phlegm.
- Developing a fever or getting the chills.
- Feeling short of breath in a way that's worse than the initial injury caused.
- A sharp, stabbing pain in your chest when you try to breathe in deeply.
Staying on top of your pain relief and diligently doing your breathing exercises are the best things you can do to defend against this serious complication.
If you are struggling with a complex rib injury and need a clear diagnosis or a second opinion, Marco Scarci Thoracic Surgery offers rapid access to specialist consultations and advanced imaging to help you get on the path to recovery sooner. You can learn more and book an appointment at https://marcoscarci.co.uk.