Breathing when your ribs are cracked can feel like glass slicing in with every inhale. Fortunately, timely pain relief and gentle breathing drills can bring real comfort. Anna, juggling work and family life, found that simple exercises paired with over-the-counter painkillers had her feeling better in just a few days.
Experiencing Fractured Rib Pain
One icy morning, Anna slipped and slammed her side against a door frame. At home, she stacked pillows behind her and took paracetamol, but every breath still stabbed sharply. Within 24 hours, she headed to A&E. Early X-rays ruled out complications like pneumothorax, and she could start pain-control exercises straightaway.
Across this guide, you’ll follow Anna as she:
Learns immediate steps to ease pain
Knows when to get imaging or urgent care
Adopts strategies from simple analgesics to guided physiotherapy
Follows long-term tips to avoid setbacks

“Prompt pain control and gentle breathing exercises prevented Anna from developing lung infections.”
Key First Aid Steps
Sit slightly leaning forward to take pressure off your ribs
Apply an ice pack for 15 minutes every two hours to reduce swelling
Use prescribed analgesics (for example, ibuprofen or codeine) as directed
Here’s a quick reference summary to keep handy:
Summary Of Fractured Rib Pain Key Points
| Aspect | Description |
|---|---|
| Symptoms | Sharp, stabbing pain when inhaling, coughing or twisting |
| First Aid | Rest in a forward-leaning position, apply cold packs, take prescribed pain relief |
| Treatment | Gentle breathing exercises, physiotherapy sessions, step-wise pain management |
| Recovery | 6–8 weeks of gradual healing with milestones for improved comfort and mobility |
Keep this overview in mind as you navigate each stage of your healing journey.
Why This Matters
Recognising the signs of a rib fracture early lets you protect your lungs and avoid problems like flail chest or pneumonia.
If you notice sudden shortness of breath, a visible change in chest shape, or blood when you cough, consult a thoracic specialist immediately.
Next, we’ll explore how a crack in your rib alters the mechanics of your chest wall and why muscle spasms add to that sharp, biting pain.
Anna discovered that by combining these straightforward steps with regular check-ins at her thoracic clinic, she was back to her normal routine far sooner than she expected. Watch the video above to see her first breathing drills in action.
Understanding Fractured Rib Pain Basics
Imagine your chest wall as a drawbridge, with each rib acting like a support beam. When one beam cracks, every breath makes the whole structure tremble. That’s why fractured rib pain often feels so raw and unrelenting.
A break in the rib doesn’t just alter the bone; it sends nearby muscles into spasm—think of them clamping down to guard the injured area. Those spasms fuel inflammation and intensify pain, so even a simple cough or sneeze can shoot sharp jolts across your chest.
Picture a snapped tent pole bending under a strong gust. While the intact poles keep the fabric taught, a broken one shifts tension to its neighbours, causing sagging sections. A fractured rib works the same way, transferring extra load to adjoining ribs and muscles.
Fractures and Breath: Force reroutes to adjacent structures
Muscle Spasm: Protective tightening magnifies sensitivity
Tissue Inflammation: Swelling irritates nearby nerves
How Rib Fractures Affect Breathing
Under normal conditions, your ribs rise and fall about 20 000 times every day—like oars rowing in perfect sync. A fracture throws that rhythm off, creating uneven chest movement.
The intercostal muscles between your ribs then spring into protective spasm. It’s your body’s way of stabilising the area, but it also makes every deep breath feel like a battle. As a result, many people resort to shallow breathing, risking poor lung expansion and further complications.
This diagram shows the typical types of rib fractures and how displacement alters rib alignment.
You’ll notice why certain breaks hurt more and why treatment varies from one pattern to another.
Initially, shock and adrenaline may mask the worst pain. But by days 3–5 post-injury, inflammation peaks, ramping up nerve irritation and causing many patients to report increased discomfort at that point.
Blunt chest trauma involving multiple fractured ribs makes up roughly 15 % of all UK trauma centre admissions—about 5 550 cases each year. Read the RIOS study here.
Why Movement and Coughing Intensify Pain
Every cough or sneeze momentarily reopens the fracture, similar to flexing a bent branch. That tiny shift can feel like bone scraping muscle and nerve endings, sparking a fierce twinge.
Leaning forward, twisting to the side or even laughter can provoke similar jolts through the chest wall. Many patients learn to hug a pillow against their ribs when they cough. While this reduces the immediate pain, over-bracing often leads to overly shallow breaths and a higher risk of pneumonia.
“Even minimal movement can transmit powerful force through a fractured rib, emphasising why pain remains intense until healing starts,” explains a thoracic surgeon.
Timeline And Statistics
A simple rib fracture typically heals in 6–8 weeks, with pain often peaking in the first seven days. However, rest alone won’t do the trick—guided breathing exercises are vital to keep your lungs fully inflated.
Key statistics at a glance:
73 % of blunt chest trauma cases are due to falls and collisions
20–25 % shorter hospital stay with early physiotherapy
5 550 multiple rib fracture admissions each year (UK data)
With these basics under your belt, you’ll better appreciate why early intervention and bespoke pain pathways are so important. In the next section, we’ll cover how to spot warning signs, decide when imaging is necessary and when to consult a thoracic surgeon.
Recognising Symptoms And When To Seek Help
Chest discomfort can mean many things, but if you’ve bruised or cracked a rib, missing the warning signs may lead to complications. Imagine drawing in a deep breath and feeling a sharp jab—this is your body’s red flag.
Tenderness on one precise spot, a grinding feeling beneath your fingertips or quick-to-appear bruising all point to a fractured rib. Spotting these clues early helps you reach the right care before issues like pneumonia or flail chest develop.
Pain on Inhalation or Coughing: Sharp twinges when you breathe in deeply
Localised Tenderness: Press the chest wall and notice a precise sore spot
Visible Bruising: Discolouration that shows up within 24–48 hours
Crepitus: A subtle grinding under the skin as fragments rub together
Differentiating Bruises And Fractures
Not all chest pain signals a break. A bruised rib often feels achy over a wider area and improves with rest and ice. By contrast, a true fracture focuses pain in one spot and flares up with every breath or movement.
Diffuse soreness that eases in a few days with cold packs
Surface-level bruising without any feeling of bone movement
Sharp, pinpoint pain that intensifies when shifting or twisting
Steady improvement after several days usually means a simple bruise
Clinical Decision Tools
Doctors lean on the STUMBL score to decide if imaging is needed. It’s a quick checklist:
Age over 65, since bones weaken with time
Anticoagulants on board, raising bleeding risks
Multiple suspected breaks, hinting at a more complex injury
Severe pain or breathing difficulties adding extra points
Early referral reduced delays and complications by 30% in an NHS audit.
If pain persists despite tablets or you struggle with daily chores, that’s your cue to seek specialist review.
Imaging And Diagnosis
An initial chest X-ray catches many—but not all—fractures. Up to 30% slip through unnoticed. When that nagging pain won’t quit, a CT scan offers a clearer picture.
First step: standard chest X-ray
Ongoing pain with a normal X-ray? Move to CT imaging
High STUMBL scores often trigger direct CT referral
In specialist centres, ultrasound can spot tiny cracks
In the UK, rib fractures represent 15% of all emergency department admissions, ranking just behind major trauma injuries. Read the full research about UK rib fracture admissions here.
Warning Signs For Urgent Care
Some symptoms demand immediate attention. If you notice any of these, don’t wait:
Sudden breathlessness or tightness that hinders speech
Chest wall deformity or paradoxical movement with each breath
Coughing up blood, suggesting lung or vessel damage
Persistent high fever or a heart rate pushing past 100 bpm
For further self-checks and tips, see our guide on how to tell if you broke a rib.
Rapid evaluation by a thoracic specialist can reduce hospital stay by 25% and boost recovery comfort.
When To Contact A Thoracic Specialist
Certain situations call for expert eyes sooner rather than later:
Patients over 65 or on blood thinners benefit from early specialist review
Worsening pain after a week or new-onset breathlessness signals a referral
Flail chest cases may need a VATS fixation to stabilise the ribs
Recognising symptoms, choosing the right tests and knowing red flags puts you on the fastest track to recovery. In the next section, we’ll cover first-aid steps and pain-control techniques you can use straight away.
Immediate First Aid And Pain Control Strategies
When a fractured rib sends a stab of pain through your chest, you need relief fast. I’m going to walk you through the first steps, just like Anna did, and point you to a quick YouTube demo that shows safe positions in action.
Back when her ribs first cracked, Anna found that leaning forward, almost like reclining in a hammock, eased the pressure. Breathing felt more natural and her lungs stayed supple, keeping stiffness at bay.
She also kept a little kit by her side—cold packs, a couple of squishy pillows and a small notebook for her pain log. That way, she never had to scramble when the ache caught her off guard.
Positioning For Comfort
Tilt your torso forward to about 30°, propping yourself up with pillows
Cradle a soft cushion against the sore side to soften the jolt of a cough
Skip tight bandages; they might limit your breath and do more harm than good
Think of your ribs like the beams of a scaffold: they need gentle support, not an iron clamp.
Breathing Drills To Keep Lungs Clear
Sit upright, ideally by a window, and inhale slowly for 3 seconds
Pause, holding the breath for 2 seconds, then let it out gently
Do this 10 times every hour, hugging a pillow against your ribs for extra comfort
“Deep breathing helps keep lung expansion steady and can cut the risk of pneumonia by 30%,” says a thoracic surgeon.
It might feel odd at first, but Anna noticed her chest stayed more flexible and free.
Monitoring Your Pain Levels
Use a simple 1–10 pain scale in a notebook. After each breathing drill or movement, Anna jotted down the time, her posture and the number she felt. Watching the numbers drop over days was a real confidence boost—and a handy guide for when to ease off.
Listening To Your Body
Learn to tell the difference between muscle soreness and sharp bone pain. If that ache jumps up by more than 2 points after a walk, stop and ice the spot. Share your pain diary with your clinician at follow-ups—it can help decide if you need extra imaging or a tweak in pain relief.
The infographic below shows how to spot pain levels, check for bruises and know when to book an X-ray.
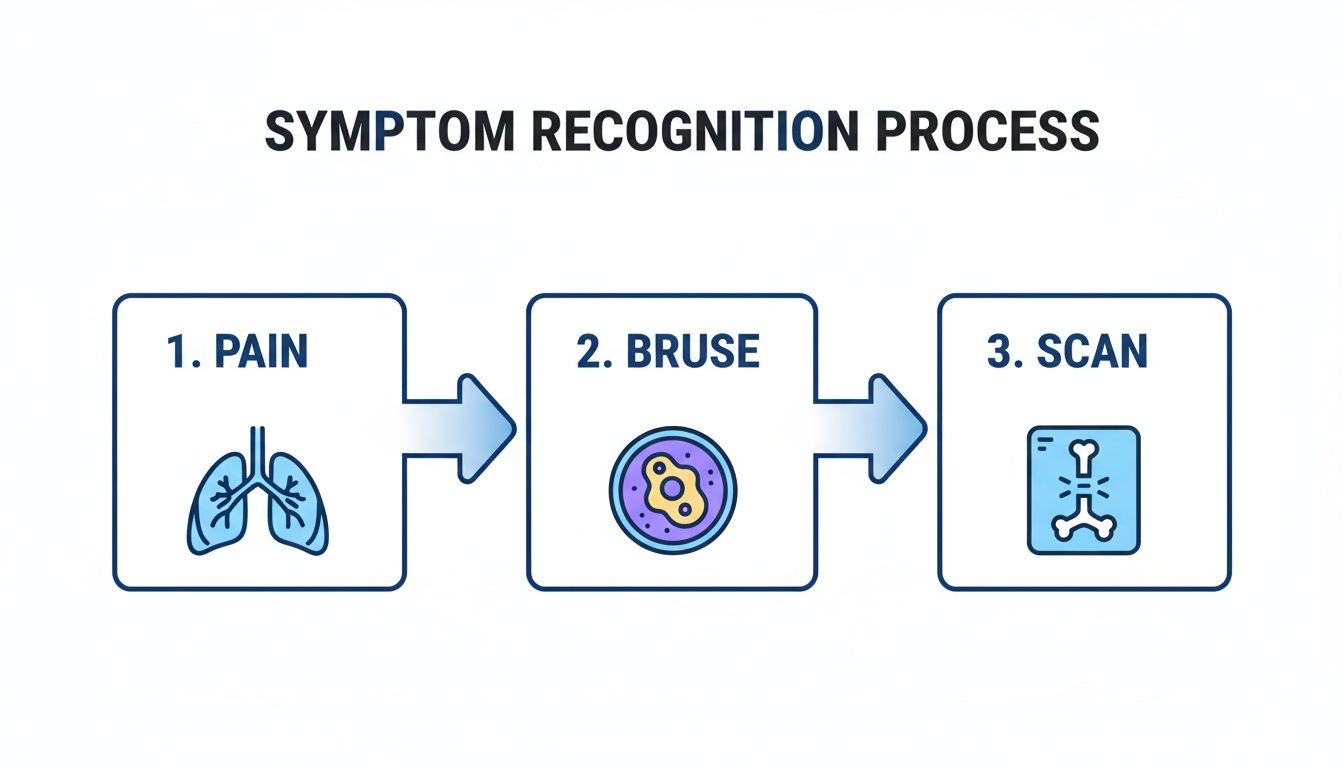
This flowchart breaks down three clear steps: recognise your pain, look for bruise patterns and seek imaging if tenderness hangs on.
Cold Packs Vs Gentle Heat
Use an ice pack for 15–20 minutes every two hours during the first 48 hours
After 72 hours, switch to a warm compress to ease tight muscles
Always layer a cloth between the pack and your skin to avoid frostbite or burns
It’s like moving from winter’s chill into the gentle warmth of spring.
Pacing And Activity
Ease back into daily life—no heavy lifting or sudden twists.
• Take short walks around the room each day
• Brace your ribs with a cushion before that cough hits
• Gradually return to chores over 2–3 weeks
Pain Relief Options
Paracetamol 500–1 000 mg up to four times a day for mild pain
NSAIDs (ibuprofen 200–400 mg) to reduce inflammation
Codeine or oral opioids under a doctor’s watch if needed
Regional nerve blocks by a specialist for targeted relief
“A multi-modal approach delivers 50% better pain control than any single drug,” notes a pain specialist.
Steer clear of tight strapping that might restrict your chest. Instead, go for breathable, supportive dressings.
Combining gentle positioning, breathing exercises and the right medications puts you in control of acute rib pain. Next, we’ll look at whether conservative or surgical management suits you best.
Always seek help without delay if pain worsens or you develop new symptoms.
Conservative And Surgical Management Options
Deciding between rest and surgery can feel like standing at a crossroads. On one side, conservative care promises gradual healing and home comforts. On the other, surgery offers faster stabilization for more serious breaks.
Consider James, a rugby coach who faced a displaced rib fracture last season. He leaned on NSAIDs, physiotherapy and gentle mobilisation. In 8 weeks, he was back to light training with manageable aches rather than sharp pain.
Here’s a snapshot from Marco Scarci Thoracic Surgery site showing care pathways and recovery milestones.

The diagram lays out each stage—assessment, pain relief and follow-up—to keep your recovery on track.
Conservative Care Highlights
Conservative management starts with multimodal analgesia to tackle pain from every angle. Think of it as a team approach:
Pain Relievers: Paracetamol and ibuprofen ease inflammation.
Nerve Blocks: Intercostal injections can give up to 12 hours of targeted relief.
Physiotherapy: Gentle stretches slowly restore chest-wall movement.
Guided Breathing: Prevents stiffness and keeps lungs clear.
Monitoring: Regular checks to track pain levels and breathing capacity.
Yet, not every case follows the smoothest path. Up to 10% of emergency department patients with rib fractures get misassigned—sent home only to return or admitted too late. Learn more about misassignment of rib fracture cases on Oxford Academic.
Comparison Of Conservative And Surgical Management
Below is a side-by-side look at the two approaches, weighing benefits, risks and who stands to gain most.
| Management Type | Approach | Benefits | Risks | Ideal Candidates |
|---|---|---|---|---|
| Conservative | Analgesia, physiotherapy, guided breathing | Low complication rate | ||
| Recover at home | Longer discomfort period | |||
| Risk of pneumonia | Mild fractures | |||
| No flail chest | ||||
| Surgical | VATS plate fixation | Rapid stabilisation | ||
| Shorter pain duration | Anaesthesia and surgical risks | Flail chest | ||
| Severely displaced ribs |
Each route has its own trade-offs. Think of conservative care as a scenic route—you’ll get there safely but more slowly. Surgical fixation is the expressway, faster but with its own tolls.
Surgical Fixation Overview
When ribs shift significantly or flail segments develop, surgery can be a game-changer. Minimally invasive VATS plate fixation uses tiny incisions and a camera to place plates precisely. On average, hospital stay shrinks by around 25% compared to open techniques.
Take Sophie, a keen cyclist who suffered a flail rib after a crash. Two days post-VATS, she noticed far less pain and could take deeper breaths. By week three, she was back on a stationary bike, easing into her recovery.
“Minimally invasive fixation can accelerate recovery and maintain pulmonary function,” says Mr Scarci.
Most surgical patients report marked pain relief by week two and resume daily activities faster. Typical stay runs 3–5 days, with chest-wall stability usually restored by week six. For more on plate fixation methods and patient pathways, visit our guide on rib fracture surgery.
Patient Story: Laura’s Rapid Recovery
Laura, a 34-year-old marathon runner, fractured two ribs in a cycling crash. After VATS plate fixation, she regained deep breathing within days and was back to gentle training by week four. Watch Laura describe her surgical recovery in my YouTube video below.
Choosing Your Path
Deciding which road to take depends on your fracture type, pain threshold and life commitments.
Conservative Care
Pros: No operation
No anaesthetic risks
Recover in familiar surroundingsCons: Longer discomfort
Strict breathing exercises
Surgical Fixation
Pros: Faster chest stabilisation
Shorter pain phaseCons: Anaesthetic exposure
Standard surgical complications
Discuss your priorities with a thoracic specialist as early as possible. A multidisciplinary team in London can tailor a plan to match your goals—whether that’s a steady at-home recovery or a quicker surgical route. Close follow-up minimizes hiccups like pneumonia or delayed displacement. Keep a pain diary, note your breathing quality and stay in touch with your care team for the best outcome.
Complications And Red Flags To Watch
Emily felt herself getting stronger in the first few days, only to find by the end of week one that taking even a shallow breath made her chest feel tight. She shrugged off the discomfort—until a sudden fever and persistent cough sent her straight back to hospital. A CT scan confirmed the culprit: early pneumonia, a frequent complication when fractured rib pain forces you into shallow breathing.
Muscle spasms around the injury often act like a cage, stopping your lungs from fully inflating. As a result, mucus can build up, setting the stage for infection or even partial lung collapse over several days. If these issues go unnoticed, they can spiral into far more serious problems.
Early Lung Complications
Hypoventilation occurs when pain stops you from breathing deeply, reducing the exchange of oxygen and carbon dioxide.
Atelectasis happens as tiny air sacs (alveoli) collapse, starving portions of lung tissue of vital oxygen.
Pneumonia may follow when fluid and secretions pool, creating the perfect environment for bacteria to thrive.
Spotting blood around the lung (haemothorax) is crucial, as accumulating fluid can quickly compress healthy tissue. In many cases, chest drainage is needed right away to restore normal breathing mechanics. Even subtle warning signs—like a racing heart or dipping blood pressure—deserve immediate attention.
Critical Red Flags
A section of ribs that moves opposite to the rest of your chest with each breath is classic flail chest and demands urgent care. A sudden spike in breathlessness or chest pain could mean a pneumothorax, often requiring emergency decompression. High fever, chills or confusion point to a systemic infection that may need intravenous antibiotics and intensive monitoring.
Take action right away if you notice any of the following:
New or worsening chest pain that doesn’t ease with painkillers—this could signal internal bleeding.
Visible chest wall deformity or paradoxical movement, suggesting unstable rib segments.
Breathlessness severe enough to stop you completing a full sentence.
Coughing up blood or pus, which can indicate lung or vessel damage.
Check out our guide on treating pneumothorax for detailed steps on chest drainage. Prompt intervention can prevent minor issues from turning critical.
Knowing these red flags helps you respond quickly and keep your recovery on track.
| Complication | Key Signs | Action Needed |
|---|---|---|
| Hypoventilation | Shallow breaths, reduced chest expansion | Step up breathing exercises, consult physio |
| Pneumonia | Fever, productive cough, chest pain | Start antibiotics, arrange medical review |
| Pneumothorax | Sudden dyspnoea, chest pain, diminished breath sounds | Urgent decompression, hospital admission |
| Haemothorax | Blood in pleural fluid, falling haematocrit | Chest drainage, possible surgical repair |
This table links each complication to its telltale signs and the swiftest remedy. Always stay in touch with your thoracic surgeon if new symptoms pop up or if your recovery stalls past the expected timeline.
Monitoring Recovery Progress
Keep a daily record of your breathing using simple tools like a peak flow metre or a pain-and-saturation diary. An unexplained spike in pain or a drop in oxygen levels should trigger an immediate check-in. Your thoracic team in London can organise fast-track assessments and imaging whenever you need it.
“Prompt detection of complications cuts serious outcomes by 30%,” says Mr Scarci.
Emily’s prompt return for chest drainage stopped her uncomplicated rib fracture from spiralling into a life-threatening emergency. By pairing vigilant self-monitoring with early specialist input, you or your loved one can avoid serious setbacks. Remember, fractured rib pain may settle on the surface while hidden problems simmer beneath. Stay alert to any changes in your breathing, temperature or chest shape—and reach out for help without delay. Stay vigilant and contact your clinic without hesitation.
Frequently Asked Questions
Anna still had questions as she eased back into life. This FAQ tackles the four issues she found most pressing, complete with practical advice and London-specific referrals.
Healing Timelines
How long does fractured rib pain stick around? In straightforward cases, you can expect your ribs to knit together in 6–8 weeks.
Factors that can speed up recovery:
Age under 65
Well-balanced diet rich in protein and vitamin C
Consistent breathing exercises
Avoiding tobacco
Anna hit her pain peak on day three but noticed real relief by week two when she started physiotherapy. A handful of patients even add zinc supplements to their routine—Anna felt a definite ease by day five.
Imaging Choices
What’s the go-to scan for a rib fracture? A standard chest X-ray catches most breaks but can miss up to 30% of hairline cracks.
Opt for a CT scan if:
Severe pain continues despite a “normal” X-ray
You score high on the STUMBL scale (age, multiple breaks)
Signs of complications appear (for example, pneumothorax)
“CT imaging reveals hairline fractures and early complications with greater accuracy,” notes a surgeon.
In London, some clinics also offer bedside ultrasound—no theatre trip or A&E wait necessary.
Home Pain Management
How can you control pain at home without reaching for strong opioids? Start with:
Paracetamol 500–1,000 mg, up to four times daily
NSAIDs such as ibuprofen 200–400 mg with meals
Ice packs for 15–20 minutes every two hours, switching to warmth after 72 hours
When to consider prescription meds? If your discomfort stays at 6/10 or higher on a simple scale after 48 hours, arrange a check-in—virtual or in person.
| Option | Benefit | Note |
|---|---|---|
| Non-opioids | Fewer side effects | Combine with other methods |
| Weak opioids | Stronger relief | Short-term use, monitored by GP |
Case Study: Tom, an IT consultant, found that adding a TENS unit to his paracetamol routine cut opioid use by 60%. Always confirm new devices with your GP.
Topical lidocaine patches or gentle TENS therapy can boost comfort and help you breathe more deeply.
Specialist Referral
When is the right moment to see a thoracic surgeon? You should seek specialised input if:
Severe pain lingers beyond two weeks
You have flail chest or multiple displaced ribs
Breathlessness or suspected pneumothorax develops
London patients can access rapid appointments through Marco Scarci Thoracic Surgery:
Virtual consultations across West, North, South and Central London
Direct CT scan scheduling via private pathways
GP referrals accepted seven days a week
Mr Scarci offers minimally invasive VATS fixation, with treatment typically starting within one week of diagnosis. Self-pay or privately insured patients can explore flexible financing options.
For expert care and fast-track support visit Marco Scarci Thoracic Surgery at marcoscarci.co.uk.