I understand that hearing the words “thymic tumour,” “thymus tumour,” or “thymoma” can feel like the ground has shifted beneath your feet. At that moment when your doctor delivers this news, the world might seem to pause, and you may find yourself flooded with fear, confusion, and countless questions racing through your mind.
You’re not alone in feeling overwhelmed. Every patient I work with describes those first days and weeks as some of the most challenging they’ve ever faced.
What I want you to know right now, at this very moment, is this: thymus cancer is treatable. With today’s advanced thoracic surgery and the expertise available, many patients go on to live whole, vibrant lives.
In this guide, you will find easy-to-understand information on thymoma and thymic cancer, thymectomy surgery, and non-surgical treatment.
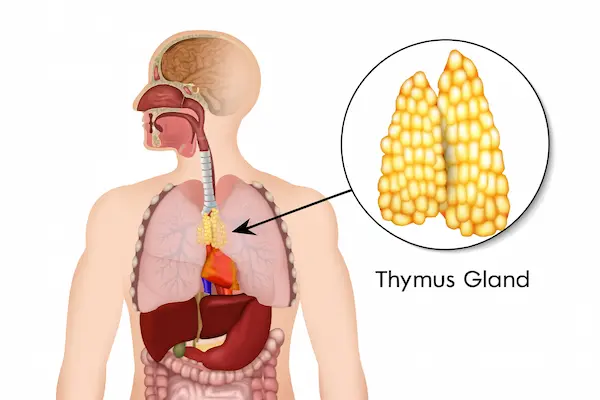
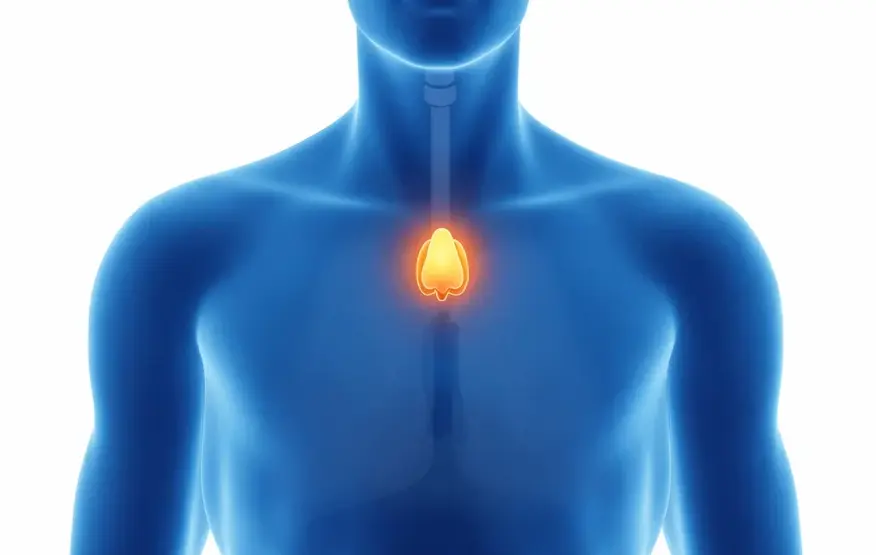
Your thymus sits quietly in your upper chest, just behind your breastbone, and can be considered the guardian of your immune system. Throughout your childhood, this gland worked tirelessly, training your T-cells – the special soldiers of your immune system – to recognise friends from foe and protect your body from infections and diseases.
As you’ve grown older, your thymus has naturally become less active, gradually shrinking. This procedure is entirely standard and part of the natural ageing process. However, sometimes the cells within this gland can begin to grow abnormally, leading to what we call thymoma.
Think of a thymoma as cancer cells that have forgotten the standard rules of growth. Unlike many other cancers you might have heard about, thymoma typically grows slowly and steadily. A thymic tumor is very different from lung cancer that you might have heard of. This slower growth pattern is actually encouraging news – it means we often have time to plan the most effective treatment approach without rushing into emergency procedures.
We classify thymomas into several distinct types, and understanding your specific type helps us tailor your treatment perfectly:




These tumours contain a mixture of different cell types, but they usually progress quite slowly. Most patients with Type AB thymoma respond very well to surgical treatment and go on to live completely everyday lives.
These can be more aggressive in their growth, but they remain highly treatable with the right approach.
For more detailed information about thymoma types and staging, visit Macmillan’s comprehensive guide to thymus cancer.
Although rare, thymic carcinoma poses significant challenges due to its aggressive nature. Rapid progression and a tendency to spread to other body parts characterize it.
Surgical resection remains a cornerstone in management, often supplemented by radiation therapy or chemotherapy to address residual cancer cells or potential spread.
Many of my patients tell me they wish they had recognised their symptoms sooner. It’s common to dismiss early warning signs, attributing them to work stress, seasonal allergies, aging, or just being “run down.” However, thymomas can create symptoms in several ways. Sometimes they grow large enough to press against nearby structures in your chest, and sometimes they can trigger your immune system to behave differently than usual.
You might notice a persistent cough that doesn’t seem related to a cold, chest pain that comes and goes, or shortness of breath during activities that never bothered you before.
Unexplained fatigue that doesn’t improve with rest, losing weight without trying, or running low-grade fevers without any sign of infection can all be signals that something needs medical attention.
About 30-50% of thymoma patients also develop myasthenia gravis, a condition that affects the communication between nerves and muscles. You might notice your eyelids feeling unusually heavy, seeing double occasionally, having trouble swallowing certain foods, or feeling like your muscles tire out more quickly than they should.
Modern imaging allows us to understand your condition precisely and plan treatment safely.
This gives us a detailed, three-dimensional map of your tumour – its exact size, location, and relationship to surrounding structures.
This is particularly valuable for showing us how close your tumour is to essential blood vessels and other critical structures. The detail we get from MRI helps us determine the best surgical technique for your specific situation.
This special scan shows how active your tumour is and whether it has spread to other parts of your body.
Your treatment follows a carefully planned and supportive pathway.
For the vast majority of early-stage thymoma patients, surgery is the best treatment option.
The goal is to remove your entire thymus gland along with the tumor and each involved lymph node – a procedure called extended thymectomy or complete thymectomy.

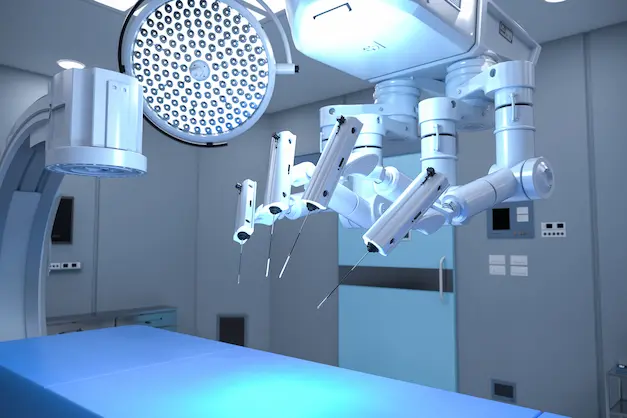
The method can be carried out either by Robotic-assisted surgery • Thoracoscopic thymectomy • VATS • Video-assisted thoracoscopic surgery • Median sternotomy • Transsternal thymectomy
Speak with a thoracic surgeon about your individual treatment plan.
In the weeks leading up to your surgical resection, you’ll work closely with your thoracic surgeon and the entire care team to ensure you’re as prepared as possible. Preparation includes:
Detailed discussions about your specific surgical plan
Pre-operative scans and blood tests to ensure optimal safety
Breathing exercises and physical conditioning to support your recovery
Clear instructions about medications, diet, and what to expect
A team prepared explicitly for your procedure will welcome you on the day of your surgery. You’ll receive general anaesthesia and sleep comfortably while your surgical team works with precision and care. Most thymoma surgeries take 2-4 hours, depending on the complexity of your case.
I will keep your family informed throughout the procedure, and as soon as surgery is complete, I will meet with them to explain how everything went.
A team prepared explicitly for your procedure will welcome you on the day of your surgery. You’ll receive general anaesthesia and sleep comfortably while your surgical team works with precision and care. Most thymoma surgeries take 2-4 hours, depending on the complexity of your case.
Pain is well-controlled with modern pain management techniques.
You’ll likely be encouraged to walk within hours of surgery.
Most patients spend only 1-2 nights in the hospital.
The nursing staff is available 24/7 to address any concerns.

Pain management during this phase is typically very manageable with prescribed medications, and most patients find they need less pain medication than they expected.
By your second and third months post-surgery, most patients have returned to all their normal activities, including sports and more intensive physical activities.
Your continued care and peace of mind.
We design your follow-up care to ensure your continued health and provide peace of mind. Regular check-ups begin at 3 months after surgery and continue every 6-12 months. These visits typically include:
Physical examinations
CT scans to monitor the surgical site
Blood tests as appropriate
Discussions about any questions or concerns you might have

These are not statistics. These are real people who stood where you stand now.

Sarah, a 42-year-old primary school teacher, still remembers the exact moment her world changed:
“When my doctor said the word ‘tumour,’ everything else became background noise. I was terrified.”
Her journey began with unexplained fatigue and a persistent cough that she initially attributed to the stress of a new school year. When symptoms persisted, her GP referred her for a chest X-ray, which revealed a mass in her chest.
“My surgeon took time to explain everything clearly. This cancer wasn’t just any cancer – it was thymoma, and it was treatable. That conversation changed everything for me.
Sarah chose robotic thymectomy, appreciating both the precision of the technique and the minimal scarring.

“I was walking the same day as my surgery. I couldn’t believe it. I went home after one night and was back to teaching within two weeks. My energy levels now are actually better than they were before my diagnosis. Two years later, I feel fantastic and rarely think about having had cancer.”
Effective communication with your healthcare team enhances the success of your thymoma treatment.
Michael, a 55-year-old architect, faced a more challenging diagnosis. His thymoma was larger and more invasive, requiring a more complex surgical approach.
“I was scared because my case was complicated, but the team coordinated everything perfectly. They even brought in cardiac specialists because my tumour was close to my heart.”
Michael’s surgery took longer than average, and his recovery was more gradual.
“The first week was tough, I won’t lie. But every day I felt a little stronger. The nursing staff was incredible, and they prepared me for exactly what to expect.”
Six months after surgery, Michael returned to his architectural practice full-time.

“Three years later, I’m completely cancer-free and back to my full life. I even took up hiking, something I’d never done before cancer. Sometimes challenges show us what we’re capable of.”

Emma, a 28-year-old marketing executive, never expected to face cancer at her age.
“I kept thinking there must be some mistake. I was young and healthy – how could this be happening to me?”
She discovered her thymoma during a routine chest X-ray for a new job.
“I had no symptoms at all. If it weren’t for that job requirement, we might not have found it for years.”
Emma chose minimally invasive surgery and was amazed by her recovery.

“I was back to work in under three weeks, and you can barely see the scars. My energy levels are actually better now than before the diagnosis. It’s like my body is working more efficiently.”
James, a 48-year-old business owner, admits he made a mistake by delaying treatment.
“I was so focused on my business that I kept putting off the doctor’s appointments. I thought I was too busy to be sick.”
When symptoms worsened, James finally sought treatment and learned his thymoma had grown larger during the delay.
“That was a wake-up call. Your health has to come first because without it, nothing else matters.”
Even with his delayed treatment, James’s outcome was excellent.

“The private treatment meant I could get back to my business quickly, but more importantly, I learned to prioritise my health. I feel better now than I have in years.”
Every story begins with a first step.Yours can begin today.
Sometimes doctors recommend it when surgeons can’t completely remove an advanced thymoma or invasive thymoma surgically, or when there’s a higher risk of recurrence. Modern postoperative radiotherapy is precisely targeted, minimising side effects while effectively treating any remaining cancer cells.
Occasionally used either before surgery to shrink larger tumours or after surgery if there are signs of more aggressive disease. Many patients are surprised to learn that chemotherapy for thymoma often causes fewer side effects than chemotherapy for other types of cancer.
The field of cancer treatment is advancing rapidly, and new immunotherapy options are becoming available. Some patients may be candidates for clinical trials testing promising new therapies.
Expert answers to common questions about thoracic surgery, recovery and what to expect.
Yes, absolutely. With early detection and appropriate surgical treatment, cure rates for early-stage thymoma exceed 95%. Even more advanced thymomas have very high cure rates with proper treatment. The key is working with experienced specialists who understand the nuances of thymoma treatment.
Doctors almost always recommend surgery when it's feasible because it offers the best chance for a complete cure. The type of surgery – whether minimally invasive or open – will depend on your specific situation, but some form of surgical removal is typically essential for the best outcome.
Both are minimally invasive approaches that use small incisions rather than wide chest openings. Robotic surgery offers enhanced precision and is particularly valuable for complex cases or when the tumour is close to critical structures. Your surgeon will help you understand which approach is best for your specific situation.
Tumour recurrence is possible but relatively uncommon, especially with complete surgical removal. The risk varies depending on the type and stage of your malignant thymoma. Doctors often recommend radiation therapy as an additional safeguard when there's a higher risk of recurrent thymoma. Your surgical team will discuss your specific risk factors and treatment options.
We understand that the financial burden of treating thymic malignancies is a genuine concern for many patients. Here's what you can typically expect:
Most private health insurance policies cover thymoma treatment, and many providers offer payment plans to make treatment accessible. Our care coordinators work with you to understand your insurance coverage and explore all available options.
About 30-50% of thymoma patients also develop myasthenia gravis, an autoimmune condition that affects muscle strength. Symptoms might include drooping eyelids, double vision, difficulty swallowing, or muscles that tire easily. If you have these symptoms, specialised testing can confirm the diagnosis. The encouraging news is that thymectomy often significantly improves myasthenia gravis symptoms.
Being open with your family about your diagnosis and treatment plan helps them support you effectively. Most families find that understanding the treatment process and expected timeline reduces their anxiety. Remember, thymoma is highly treatable, and most patients return to a completely normal life.
One of the most remarkable things about thymoma treatment is how completely most patients return to their everyday lives. The surgery addresses the cancer, and for many patients with associated myasthenia gravis, symptoms improve dramatically or disappear entirely.
Patients often tell us they feel better after treatment than they did before diagnosis. Whether it's increased energy levels, better breathing, or improved muscle strength, the benefits of removing the thymoma extend far beyond just treating the cancer.
You have every reason to feel hopeful about your future. With world-class medical expertise, advanced surgical techniques, and comprehensive support systems, you're in the best possible position to overcome this challenge and return to living the whole, vibrant life you deserve.
If you're reading this guide, you've already taken an essential step by seeking information and taking an active role in your healthcare. That initiative and determination will serve you well throughout your treatment and recovery.
The path ahead might seem daunting right now, but remember: you're not traveling it alone, and you're heading towards healing. Thousands of patients have walked this path before you and emerged stronger, healthier, and grateful for the opportunity to reclaim their lives.
Your story of overcoming thymoma is about to begin. Like Sarah, Michael, Emma, and James, you too can face this challenge with courage, receive expert treatment, and return to the life you love – perhaps with an even deeper appreciation for health, family, and the precious gift of each day.
The first step is to schedule an initial consultation. From that moment forward, expertise will guide every step, compassion will support every step, and one goal will focus every step: getting you back to your life, healthier and stronger than before.
You've got this, and I have got you.
Contact me today to schedule your consultation. Your journey to better health starts with a single phone call.